Idiopathic Anal Fistula: Fistulotomy or Fistulectomy?
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Elroy Patrick Weledji
Abstract
A fistula has a primary tract and may have secondary extensions. Complete eradication of both may lead to cure. Lay- open (fistulotomy) is the most certain treatment where it is possible and when the risks have been properly explained and accepted. Anterior fistulas in women are dangerous and should only rarely be laid open. The technique of fistulectomy, which excises rather than incises the fistula track, has been criticised on the basis of the greater tissue loss leading to delayed healing. However, fistulectomy by a core-out technique rather than excision of the track have several advocates. The paper discussed the natural history of the idiopathic anal fistula and the pros and cons of these two common modes of treatment.
Keywords: Fistulotomy; Fistula; Eradication; Idiopathic anal; Chronic anal fistula; Crohn’s disease
Abbrevations: AES: Anal Endosonography;STIR: Short Tau Inversion Recovery; LIFT: Ligation of the Intersphincteric Fistula Tract, VAFT: Video-Assisted Anal Fistula Treatment
Introduction
Anorectal sepsis is common, presenting as either an acute abscess or a chronic anal fistula. The majority of cases are dealt with minimum complications, but a small minority may present a major challenge to both sufferer and surgeon. The majority are classified as non-specific, idiopathic or cryptoglandular in which the diseased anal gland in the intersphincteric space is considered central [1,2]. However, fistulas may be seen in association with Crohn’s disease, tuberculosis, pilonidal disease, hidradenitissuppuritiva, lymphogranuloma venereum, presacral dermoids, rectal duplication, actinomycosis, trauma and foreign bodies [1]. An important association is malignancy which may manifest itself as a discharging opening on the perineum from a pelvic source, but which may also arise in long-standing fistulas, either cryptoglandular, as part of perianal Crohn’s disease, or even in hidradenitis suppurativa. The exact incidence of idiopathic anal fistula in the general population is not known, as most data come from hospital analysis in tertiary referral centres, which attract the more difficult cases. The most accurate information come from Scandinavia of between 8.6 and 10 per 10,000. All reported series have demonstrated a male pre-dominance of between 2:1 and 4:1 for reasons that are unclear. It most commonly afflicts people in their third, fourth or fifth decades [3,4] with a peak incidence at a lower age in Nigerians and in African Americans [4]. Whether bowel habit may be influential is unclear. Diarrhoea may allow easier access of bacteria to the anal glands, especially in infants. Hard stools may be implicated by their abrasive passage through the anal canal.
Aetiology
Eissenhammer[5] considered all non-specific abscesses and fistulas to be the result of extension of sepsis from an intramuscular anal gland (situated in the intersphincteric spaces), the sepsis being unable to drain spontaneously into the anal lumen because of infective obstruction of its connecting duct across the internal sphincter.Parks [6] proposed that, should the initial abscess in relation to the intersphincteric anal gland subside, the diseased gland might become the seat of chronic infection with subsequent fistula formation. The fistula is thus a granulation tissue-lined track kept open by the infective source, which is the abscess around a diseased anal gland deep to the internal sphincter. However, a proportion of cases of acute sepsis have nothing to do with fistula and some common fistulas e.g. superficial fistulas and those arising from a chronic anal fissure have an aetiology separate from that postulated by Parks.Infection and its effective drainage are the primary problems in the acute stage, and failure to treat secondary extensions and abscesses adequately will lead to recurrence.Idiopathic fistulas may also persist if they become (at least partly) epithelialised[7,8], a factor responsible for failure of healing of fistulas at other sites in the body [9]. The presence of epithelium and the local production of antimicrobial peptides may explain the relative paucity of organisms found in chronic fistulas [10].
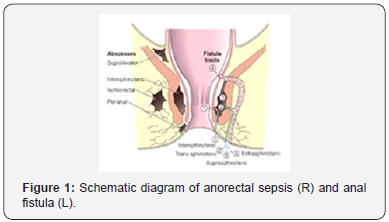
Spread of sepsis from an acutely infected anal gland may occur in any of the three planes, vertical, horizontal or circumferential [6]. Caudal spread is the simplest and most usual way by which infection is thought to disseminate to present acutely as a perianal abscess. Cephalad extension in the same space will result in a high intermuscular abscess or a supralevator pararectal (syn. Pelvirectal) abscess, depending on the relation of the sepsis to the longitudinal muscle layer. Lateral spread across the external sphincter will reach the ischiorectal fossa, where further caudal spread will result in the abscess pointing at the skin as an ischiorectal abscess; upward spread may penetrate the levators to reach the supralevator pararectal space (Figure 1).
Circumferential spread may occur in any of the three planes, intermuscular (intersphincteric) but with no restriction to a level beneath the anorectal ring), ischiorectal or supralevator[11]. All those conditions which Eisenhammer [12] considered not to be of cryptoglandular origin he placed into the miscellaneous group of acute anorectal non-cryptoglandular non-fistulous abscesses. These included the submucous abscess (arising from an infected haemorrhoid, sclerotherapy or trauma), the mucocutaneous or marginal abscess (infected haematoma), the perianal abscess (follicular skin infection), some ischiorectal abscesses (primary infection or foreign body) and the pelvirectalsupralevator abscess originating in pelvic disease.
Clues to the aetiology of perineal sepsis may be gleaned from microbiology of the drained pus [13,14]. If skin organisms alone are cultured and the acute abscess adequately drained recurrence should not occur, and a fistula will not result. If gut organisms are cultured, it is probable but not inevitable that there is an underlying fistula. The results of microbiology are therefore sensitive (100%) but not totally specific (60-80%) [1,13,14]and of course are not available at the time of initial surgery.
Classification of Anal Fistula
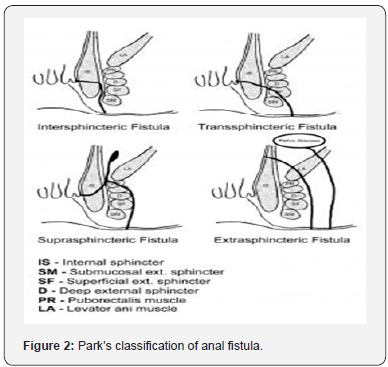
The cryptoglandular hypothesis is central to the classification, which holds firstly that the majority of fistulas arise from an abscess in the intersphincteric plane and secondly that the relation of the primary track to the external sphincter is paramount in surgical management. Four main groups exist: intersphincteric, trans-sphincteric, supra-sphincteric and extrasphincteric[11] (Figures 1&2). These groups can have secondary extensions or tracks.Intersphincteric fistulas, constituting 45% of cases in the original St Mark’s series are usually simple; although some may have a high blind track, or a high opening into the rectum or no perineal opening, or even high pelvic extension, or even arise from pelvic disease. Trans-sphincteric fistulas (29%) have a primary track that passes through the external sphincter at varying levels into the ischiorectal fossa. It may be uncomplicated, consisting only of a primary tract or can have a high blind tract that may terminate below or above the levator ani muscles. Suprasphincteric fistulas (20%) run up to a level above puborectalis and then curl down through the levators and ischiorectal fossa to reach the skin. Extrasphincteric fistulas (5%) run without relation to the sphincters and are classified according to their pathogenesis. In addition, sepsis may spread circumferentially in any of these three spaces: intersphinctericc, ischiorectal or pararectal [1,11].
Principles of Fistula Surgery
A full history and examination including proctosigmoidoscopy are essential in all cases to exclude any associated conditions. Clinical assessment involves five essential points, enumerated by Goodsall& Miles [15]at the end of the 19th century:
a) Location of the internal opening,
b) Location of the external opening,
c) Course of the primary track,
d) Presence of secondary extensions
e) Presence of other diseases complicating the fistula.
The relative positions of the external and internal openings will indicate the likely course of the primary track, and the presence of any palpable induration, especially supralevator, should alert the surgeon to a secondary track [1,15-17]. The distance of the external opening from the anal verge may assist in differentiating an intersphincteric from a trans-sphincteric fistula; the greater the distance, the greater the likelihood of a complex cephalad extension [1,4,16,17].Goodsall’s rule generally applies in that the likely site of the internal opening can be predicted by the position around the anal circumference of the external opening (Figures 3a&b).It states that if the perianal skin opening is posterior to the transverse anal line, the fistulous tract will open into the anal canal in the midline posteriorly, sometimes taking a curvilinear (horseshoe-shaped) course. A perianal skin opening anterior to the transverse anal line is usually associated with a radial fistulous tract following a simple, direct course [15].


Exceptions to this rule include anteriorly located openings more than 3 cm from the anal verge (which may be anterior extensions of posterior horseshoe fistulas) and fistulas associated with other diseases especially Crohn’s and malignancy. Previous surgery leads to scarring and deformity, as well as the creation of unusual primary tracks make clinical assessment difficult. Anal endosonography (AES) may assess the integrity of the sphincters and the diagnostic accuracy in imaging anal sepsis is increased with the use of hydrogen peroxide injected into fistulous tracks to act as a contrast medium.By providing high soft-tissue resolution the endocoil receiver MRI is the gold standard for assessing anorectal sepsis. Anal sepsis appears on MRI as areas of very high signal, which enhance with the administration of the intravenous contrast agent gadolinium Definition is further increased with the use of the STIR(short tau inversion recovery) sequences to suppress the signal returned by fat [18,19].
Milligan, et al. [20] stressed the importance of the anorectal ring in fistula surgery. If this ring be cut, loss of control results, yet as long as the narrowest complete ring of the puborectalis muscle remains control is preserved. In the UK most, anal fistula surgery is performed with the patient in the lithotomy position, although the prone jack-knife position is gaining popularity. The St Mark’s Hospital fistula operation sheet provides an excellent standardised format for documentation both by description and by illustration [21].
Surgical Treatment
The multiplicity of techniques designed to preserve sphincter function and at the same time eradicate fistula pathology reflects their relative lack of success. A degree of caution and scepticism may be appropriately apportioned when assessing results of the various approaches towards complex fistula such as setons, advancement flaps, biological agents (fibrin glue, bioprosthetic plugs), LIFT (ligation of the intersphincteric fistula tract, VAFT (video-assisted anal fistula treatment)[21-26], since
i. The patient populations may be markedly different,
ii. Fistula classification may be variable,
iii. Reports of successes may not be tempered by honest reporting of failures,
iv. Reports of success have not always been accompanied by reports of changes in continence,
v. The use of adequately powered prospective randomised trials is perhaps unachievable, because of individual fistula (and sphincter) variability and individual surgeon preference and skill,
vi. Follow-up may be inadequate.
Fistulotomy
Fistulotomy (laying open) and allowing to heal by secondary intention from beneath upwards remains the surest way of eliminating an anal fistula. All lay-open procedures divide some of the internal sphincter, so patients should be warned of a 1 in 4 chance of flatus incontinence and mild mucus leakage. Its application should, in the first instance, be restricted to situations where a significant degree of incontinence would not result [21,27]. Marsupialisation, i.e. suturing the divided wound edge to the edges of the curetted fibrous track, results in a smaller wound and faster healing [28,29].
Intersphincteric and low trans-sphincteric tracks are probably best treated by this method, but the decision whether to lay open rests on the skill and experience of the surgeon and informed advice to the patient. High trans-sphincteric (especially anterior tracks in women) and suprasphincteric tracks should not be treated by one-stage fistulotomy. Anterior fistulas in women are dangerous and should only rarely be laid open [27]. In the field of sphincter and continence preservation the’ loose’ seton (a thread loosely tied as a marker of a fistula tract when its exact position and level in relation to the external sphincter is unclear at surgery, perhaps because of scarring from previous surgery or because of the depth of sphincter muscle relaxation under anaesthesia) is useful. It can be used in three ways: to preserve the entire external sphincter whilst draining an acute sepsis; to preserve part of the voluntary muscle; or as part of a staged fistulotomy in order to reduce the consequences of division of large amount of muscle in one procedure.
The key points of a staged fistulotomy are the amount of muscle divided at each stage and the time allowed for fibrosis to develop between the divided muscle edges before a further length of sphincter is divided [30-32]. Postoperatively, the wounds are managed by daily digitation and irrigation. At outpatient review, if there is evidence of good healing both of the wounds and around the seton, the latter is removed at 2-3 months. Any suspicion of ongoing sepsis requires repeat examination under anaesthesia.Secondary extensions from the primary track can be dealt with in two ways. It could be widely laid open to allow maximal drainage, which is followed by healing by secondary intention. As long as the external sphincter is intact, the residual scarring after healing is remarkably little.
In the USA, the use of incisions, counter incisions and the placement of encircling drains left in for 2-4 weeks will render more rapid healing and less deformity.It is important to note that, fistulotomy and immediate reconstruction of the divided musculature, and with primary closure rendered an 88% healing rate by 2 weeks [33]. There was a 4% recurrence rate and all patients were satisfied. However, these fistulas were mosly low intersphincteric or simple trans-sphincteric. The technique applied to a small cohort of patients with recurrent complex fistulas gave impressive results in terms of healing rates, manometric and functional outcomes, and with no dehiscence of the reconstituted sphincter [34]. It yielded equivalent results with advancement flap repair [35].
Fistulectomy
The technique of fistulectomy, which excises rather than incises the fistula track, has been criticised on the basis that the greater tissue loss leads to delayed healing [36]. However, fistulectomy by a core-out technique rather than excision advocated by Lewis [37] has the following advantages:
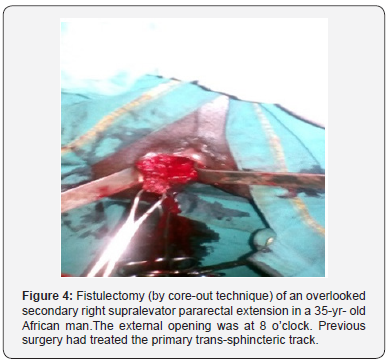
a) The precise course of the track is more accurately determined by core-out under direct vision (Figure 4) and does not involve the passage of probes along the track and thus creation of false tracks.A Probe is used only to open the external opening and assist in inserting a stay suture around it;
b) Coring out the primary track reduces the risk of missing secondary tracks, which are seen astransected granulation tissue and which may be followed by the same technique (Figure 4).
c) The relation of the primary track to the external anal sphincter may be correctly ascertained before any sphincter muscle is divided;
d) A complete specimen is available for histology.
Once the track has been cored out, from the external towards the internal opening using either scissors or cautery dissection, the decision as to whether the tunnel is left after the core-out can be safely laid open is made. For a non-recurrent single transsphincteric track, a simple anatomical closure of the cored-out tunnel, with mucosal closure and closure of the holes in the muscles was recommended by Lewis [38], following only one recurrence in his low fistula’s series.However, a temporary colostomy was raised in four of 32 patients with high transsphincteric or supra-sphincteric fistulas and there were three recurrences. In the case of recurrent or more complex fistulas the adoption of other sphincter conserving methods such as loose setons and staged fistulotomy, or VAAFT [16,26,32], were recommended since excessive scarring and the larger defect created by coring-out makes simple anatomical closure inappropriate [30,38]. Advancement flaps are intuitively attractive but practically uncertain. Glue is only rarely effective. Bioprosthetic plugs are more attractive but long-term results of healing validated by MRI are awaited [21]. Marsupialization of fistulectomy wounds will also improve and allow healing from below-upwards and decrease bleeding [29].
Conclusion
A fistula has a primary track and may have secondary extensions. Complete eradication of both will lead to cure. Fistulotomy (lay-open) is the most certain treatment where it is possible and when the risks have been properly explained and accepted. Fistulectomy by a core-out technique has certain advantages but not for the recurrent or complex fistulas where the excessive scarring and larger defect created makes simple anatomical closure inappropriate.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment