Unexpected Delayed Rectal Perforation after Endoscopic Submucosal Dissection
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Valerii Giorgio
Abstract
Superficial gastrointestinal neoplasia may be removed endoscopically.ESD (Endoscopic submucosal dissection) isaneffectiveandsafe procedurewhich allows “en bloc” resection of superficial gastrointestinal lesions.The most common adverse events ofESD are perforation and bleeding.Late perforation are rare and occur in 0.22% according to literature.We report a case of delayedrectal perforation, occurring 16days after ESDof a 65 x 35-mm laterally spreading tumor (LST) nodular mixed type(G-MIX), ofthe rectum.The perforation wascompletely unexpected because ofabsence of post-ESD risk factors and the long period of wellness of the patient after the procedure.
Keywords: Colorectal lesion; Endoscopic Submucosal; Dissection; Delayed rectal perforation
Abbrevations:LST: Laterally Spreading Tumor; G-MIX: Nodular Mixed Type; EMR: Endoscopic Mucosal Resection; ESD: Endoscopic Submucosal Dissection; NBI: Narrow Band Imaging; TEM: Trans analEndoscopic Microsurgery
Introduction
Superficial gastrointestinal tumor may be removed endoscopically.Endoscopic mucosal resection (EMR) is one ofthe most usefulendoscopic technique toremove gastrointestinal superficial neoplasia,endoscopic submucosal dissection (ESD) is a new endoscopic technique to overcome EMR limits (en bloc resection of lesions larger than 20 mm or non-lifting lesions).
ESD is nowadays considered an effective and safe endoscopic technique.Colorectal ESD can be consideredto perform en bloc resection of the large lesions (>20 mm)or to ensure an accurate histopathologic evaluation and a radical treatment with lower risk of relapse[1].
ESD, however,requires greater skill, longer operation time and higher costs than EMRwitha higher incidence of serious adverse events such as immediate (4.2%) or delayed (0.22%) perforation[2]. We report a case of laterectal perforation,16daysafterendoscopic removal ofa 65 x 35-mm laterally spreading tumor (LST) G-MIX(nodular mixed type) in the rectum using a standard ESD technique.
Case Report
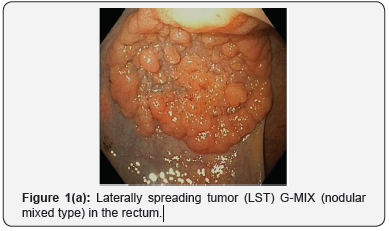
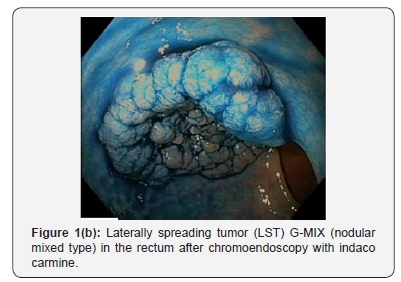
An 82-year-old womanwithout relevant past medical historyexcept for high blood pressure on medication, underwent colonoscopy due to the occurrence of rectal bleeding; colonoscopy revealed a rectalLST G-MIX,starting 15cm from the anal canal and extending proximally, measuring 65 x 35 mm endoscopically(Figure 1a).Virtualchromoendoscopy (Narrow bandimaging NBI) and after Indigo carmine (0.4%)were performed in order to characterize and to establish the feasibility for endoscopic treatment of the lesion(Figure 1b).The lesion had a type IVpit pattern (Figure 1b), according to Kudo classification.ESD was performed underdeep sedation with propofol.Submucosal injection was performed with Glicerol 10% and sodium chloride 0.9% mixed with Adrenaline (1:10000) andindigo carmine..
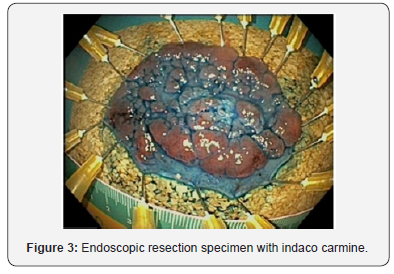
Subsequently, circumferential incision to access the submucosa was performedbeginning from the mucosa proximal to the tumor. Local injections were repeated with subsequent dissection of the submucosaover the muscolar layer todistal side of the tumor(Figure 2). Submucosal dissection was performed with the Dual Knife (Olympus, Tokyo, Japan).Coagrasper (FD- 410LR; Olympus) was performed to coagulate large visible vessels or bleeding sites.Finally, thesubmucosal layer was dissected, and the tumor was resected en bloc (Figure 3).
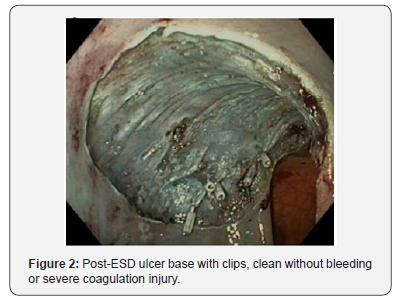
The procedure time required for ESD was 70 minutes. Noimmediate procedure-related complications were noted.To prevent late bleeding and perforation, clipping of visible vessel with hemoclip(Olympus, Tokyo, Japan) was4performed.
The tumor measured 65×35 mm (Figure 3).Microscopic examination revealed a tubulovillous adenoma with high-grade of dysplasia,vertical and lateral margins were negative (Figure 3).There was no evidence of histological damage to themuscolar layerby any cautery effect or air.The following morningher white blood cell count wasnormal.The first follow-up was scheduled, with phone contact, after 10days.
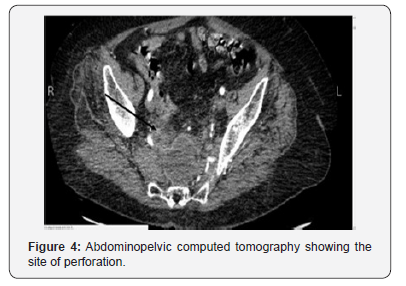
However, 16days after ESD the patient complainedmild abdominal pain andfeverwith a slight leukocytosis. Ultrasonography revealed free fluid with specks of air in peritoneal cavity. CT scan of the abdomen and pelvis revealedintraperitoneal air and fluid inthepelvic region andmesorectum-mesosigmoid with anorganized collection in the presacral space and irregularities at theendoscopic resection site(Figure 4).
Broad spectrumantibiotics were administered,and CT-guided drainage of the pelvic collection was performed.CT-scanwas performed 72hours after the drainage, percutaneous drainage of the collection wasnot effective and due to the persistence of fever and increase of white blood cellthe patient underwent surgery andaloop colostomy of the transverse colon was performed after thorough irrigation of the peritoneal cavity.Post-operative course was uneventful, and the patient was discharged after 7 daysfrom surgery.
Discussion
Colorectal ESD seems to be an extremely safe andeffective procedure (1) providingen bloc resection with accurate histopathologic assessment particularly for lesions larger than 20 mm,with a relatively low risk of recurrenceand88% R0 resection rate[3,4].Transanal endoscopic microsurgery (TEM) procedures have ahigherrecurrence ratethan ESD(5.2 % versus2.6 %)[5,6]. The most common adverse events after gastrointestinal ESD are immediate or delayed perforation and major bleeding[1].
Risk factors for ESD perforation are well known (fibrosis, lesion diameter(i.e., ≥50 mm), low endoscopist experiencein ESD) [7].
The reported ratesof immediateand delayed major bleeding, after colorectal ESD, are 0.75% (95%CI, 0.31–1.8 %) and 2.1% (95% CI, 1.6–2.6 %); immediate perforation arereported in4.2% of the cases (95% CI, 3.5–5.0 %)whereasdelayed perforationisvery rare (0.22%, 95% CI, 0.11–0.46 %)[5]and in one-third of the cases diagnosedwithin 24 hours[4].Thirtystudies reported delayed perforation after colorectal ESD in 3887lesions[4].
Abdominal pain, fever and an inflammatory responseare signs and symptoms of supposed delayed perforation, often caused by an electrical or thermal injury after electrocoagulation,also namedCoagulation Syndrome (CS)[8,9].The diagnosis of delayed perforation is performed byCT-scan with contrast[8].CS is an electrocoagulation injury to the muscolaris propria and serosa during polypectomy, EMR orESDthat induces a transmural burn without perforation[7,8,10]. Delayed perforationcaused by CSisusuallysevereand often requiressurgery.3In the current case the rectal perforation was diagnosed16 days after ESD ofan LSTin the rectumand furthermore unexpected.
The patientwas healthy, and the only risk factor washypertension but well controlled with medication;there were no ESD-associated risk factors for perforationexcept tumor size (>50 mm), no severe coagulation damage was apparent at the post- ESD ulcer base.Therefore, endoscopists should closely evaluate patient also after clean ESD, and in case of suspiciousabdominal pain perform CT scan with contrast.Delayed perforation,after 16 daysfrom an uneventful procedure,is a rare but possible serious adverse eventof ESD.
Conflict of Interests
Guido Costamagna has received grant/research support from Olympus Japan, is a member of advisorycommittees or review panels for Cook, Inc., Boston Scientific Corp., and Taewoong Medical, Inc., and hasbeen a speaker and teacher for Boston Scientific, Corp. and Given Imaging.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment