Effectiveness of using Low-Osmolarity Water-Soluble Contrast in the Evaluation of Intestinal Obstruction with Conservative Management
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Quitzia Libertad Torres Salazar
Abstract
Introduction: Intestinal occlusion represents a frequent cause of medical attention in the emergency department, within the current management guidelines it is well established that conservative treatment should be used as the first option. Gastrographic® has been recommended to be used as a contrast agent as a predictor of successful conservative management; however, it is not usually available for use in public hospitals in our country.
Objective: To determine whether oral low-osmolarity water-soluble contrast [LOWS] is useful in identifying patients with bowel obstruction who will have a good response with conservative management.
Material and Methods: Prospective, non-randomized, cohort study conducted in patients over 18 years of age, who presented with a diagnosis of intestinal obstruction. A nasogastric tube was placed for gastric emptying and intestinal decompression. After 6 hours, improvement was assessed by the decrease in nasogastric tube output and contrast medium was administered. Bolus LOWS 50cc were used and followed up radiologically. Surgical management was considered lacking contrast 24 hours after administration.
Results: In 41 cases we observed adequate passage of contrast and in 7 cases it did not reach the colon, in which case surgical exploration was indicated. Of the 41 patients with adequate clearance, 7 underwent surgery because of continued symptomatology. A PPV of 100% and NPV of 82.92% were calculated. The rate of complications is closely related to the need for surgical intervention, the degree of contamination of the abdominal cavity and hospital stay, there were no adverse events associated with the use of LOWS.
Keywords: Intestinal Obstruction; Water soluble contrast; Predictive value
Introduction
Intestinal obstruction is among the conditions most frequently encountered by the surgeon, accounting for approximately 15% of surgical admissions to the emergency department [1]. Also called intestinal occlusion syndrome, it has multiple causes, which the surgeon will have to identify. This, by the clinical history and the clinical condition of the patient, to reach a diagnosis and choose the appropriate management required by the patient [2]. The lack of a standardized protocol that indicates which is a best management and when to opt for surgery without presenting complication data, causes in patients with intestinal occlusion. Likewise, it also causes a delay in decision-making, sometimes prolonging conservative management and postponing surgical intervention with the risk of presenting complications such as ischemia and perforation. In most public hospitals in our country, the Gastrographic® contrast medium recommended by international guidelines is not available [3]. Therefore, a study that determines the usefulness of low osmolarity water-soluble contrast [LOWS] [which is regularly available] to predict the evolution of these patients, would allow us to standardize the use of this study during the evaluation of the patient with intestinal occlusion, safely, enabling timely and appropriate management.
Material and Methods
A prospective, longitudinal cohort study was designed, with nonrandomized sampling by consecutive cases. Performed in patients over 18 years of age who were admitted to the emergency department with clinical symptoms of intestinal obstruction. The sample size was calculated using the formula for diagnostic and prognostic studies, with a confidence level of 95%, a power of 80% and an expected PPV of 95%, with a minimum of 48 subjects to be included. This study was approved by the Ethics and Research Committee of the Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, of the State of Jalisco, and each patient and witness signed the letter of informed consent. The study included men and women, over 18 years of age, who arrived at the emergency department with a clinical picture compatible with intestinal obstruction; patients who had been admitted with surgical criteria or who reported allergies to the contrast medium were excluded from the study. On admission, a nasogastric tube [NGT] was placed in each patient to facilitate gastric emptying and intestinal decompression. Subsequently, intravenous hydro electrolytic resuscitation was administered and criteria for surgical intervention were evaluated. Once the selection criteria were met, the patient was left under observation for 6 hours to identify if there was improvement, reflected by a decrease in symptoms and a decrease in NGT expenditure. At that time, 50 ml of LOWS was administered as a bolus through the catheter, with subsequent clamping to prevent it from draining out of the gastrointestinal tract. Follow-up at 12 and 24 hours was done with plain abdominal radiographs to evaluate the passage of contrast through the colon. The criterion for surgical management was the absence of contrast 24 hours after administration or the presence of the following: increased pain, abdominal distention, signs of peritoneal irritation, elevated NGT output, fever or increased white blood cell count. All data were analyzed with the SPSS ver.25 Spanish statistical program.
Results
The evolution of 48 patients was analyzed; in 41 cases we observed adequate passage of the contrast medium and in 7 cases it did not reach the colon and surgical exploration was indicated. Of the 41 cases, 7 [17%] received surgical intervention due to continued symptomatology 34.3±14.8 hours after hospital admission and 14.612.6 hours after contrast application. The clinical and demographic characteristics are shown in table 1.
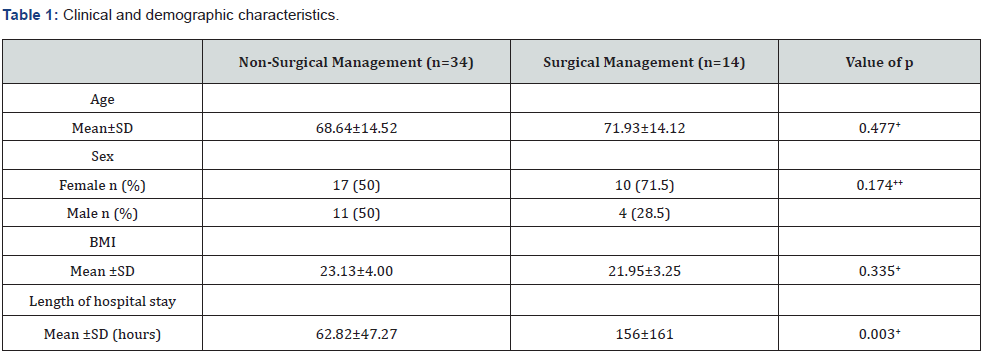
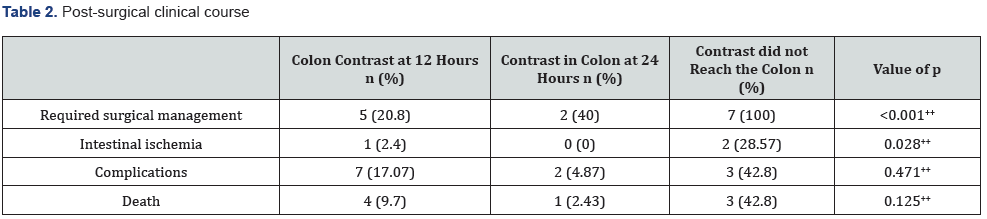
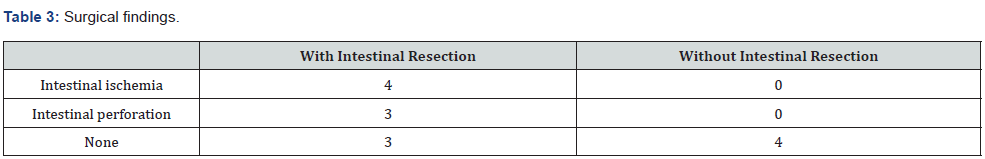
The clinical post-surgical evolution of the group that merited surgical management was compared, finding a significant difference in the need for surgical management in patients who did not present a transit of contrast up to the colon level in radiological studies at 24 hours (Table 2). Of the 14 patients who underwent surgery, 10 [71.4%] of them received a bowel resection [3 of the group in which the contrast did not clear at the colon level within the first 24 hours] and 12 [85.7%] had postoperative complications. Of the 10 intestinal resections, in 7 [70%] large bowel resection was performed, either at the ascending [3], descending [3] or sigmoid [1] colon level. Surgical findings are shown in table 3.
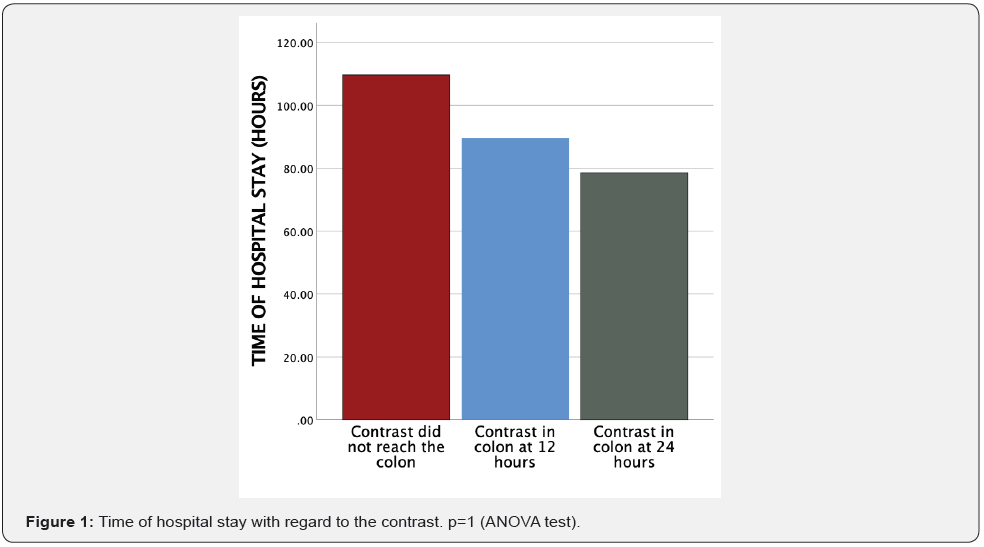
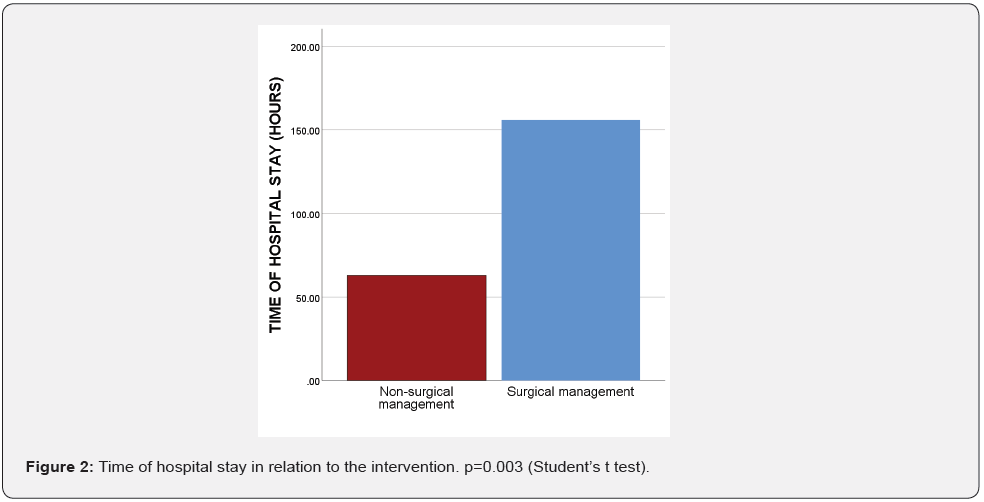
Regarding the length of stay of the patients, no statistically significant difference was observed in the length of stay with respect to the contrast time (Figure 1). However, there was a difference in the length of stay between patients who underwent surgery and those who did not (Figure 2).
To evaluate the use of LOWS as a predictor of the need for surgical intervention, we performed the test to determine the positive and negative predictive values [PPV and NPV], taking into consideration the data in Table 4, obtaining a PPV of 100% and an NPV of 82.92%. Using these same data, we were able to evaluate the sensitivity and specificity of this predictive tool, obtaining 50% sensitivity and 100% specificity.
Discussion
In this study, it was found that the use of orally administered LOWS allowed the detection of 100% of patients who would not resolve with conservative management with a PPV of 100% and NPV of 82.92%. It should be noted that of the 7 cases found that the contrast did not clear the colon within the first 24 hours after administration, 6 of them presented complete mechanical obstruction at the small bowel level: 2 of them with established intestinal compromise that required intestinal resection and 4 cases only required adhesiolysis to free the site of obstruction.
Evaluating hospital stay, a difference of 2.6 vs. 6.5 days was found between the conservative and surgical management groups. On 3 occasions, one patient presented intolerance to the oral route prolonging his stay, in the rest of the cases the diet progressed after 12 hours of the contrasted study in which contrast was evidenced at the colon level and without clinical data of intestinal obstruction. One patient with adequate contrast clearance in the colon was diagnosed with Crohn’s disease. This patient tolerated the diet after 72 hours and his stay was prolonged up to 10 days for diagnostic studies, which increased the mean in days for the non-surgical group. Similar data have been reported in another study in which the mean hospital stay for the non-surgical group was 2 days for those who presented contrast in the colon in the first 12 hours, while for the group that presented it between 12 and 24 hours its mean in days was 4.5; while for the group that underwent surgery it was 8 days [4,5].
The rate of complications is closely related to the need for surgical intervention, the degree of contamination of the abdominal cavity and the hospital stay. Our complication rate was 66.66% for the surgical group vs. 11.76% for the conservative group, presenting in-hospital infections such as pneumonia, pulmonary thromboembolism, and acute renal failure secondary to septic state.
Discarding the patients who underwent surgery for colon pathology, of the remaining 41 patients, 7 showed total obstruction and underwent surgery, with a success rate of 83% for conservative management. This result is similar to that previously described with high osmolarity water-soluble contrast, reporting a 77% success rate of conservative management [4,5].
One of the limitations of our study is the number of patients collected, since increasing the sample size would help us to reach a more generalized conclusion. Another point to consider is the difference in the criteria used by physicians to initiate an oral diet and discharge patients due to the aforementioned issues. A more accurate elaboration of the service protocols will allow standardizing the treatment in a homogeneous way, decreasing the time to start the diet and, therefore, the length of hospital stay.
Conclusion
These results suggest that it is possible to identify patients with total obstruction from those with partial obstruction using LOWS for early intervention.
Declarations
Ethics approval and consent to participate: Autograph consent was obtained from the patient for the presentation and publication of her case. This study was evaluated and approved by the research ethics committee of the Valentín Gomez Farias Hospital.
Consent for publication: Written informed consent was obtained from all the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of data and materials: The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ Contributions
DENN, JLVS, OUAP, LMGB, GEC, JECA, QLTS were involved in the patient’s care. All authors have contributed substantially to collecting data, revising the article, and having given necessary intellectual inputs. All authors read and approved the final manuscript.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment