Use of Vedolizumab in Preventing Postoperative Recurrence of Crohn’s Disease and Previous Anti-Tnf Alfa Failure: A Case Report
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Annalisa Pasetti
Abstract
Vedolizumab (VDZ) is a monoclonal antibody that inhibits the interaction of α4β7 integrin with mucosal addressing cell adhesion molecule-1 (MAdCAM-1). Although it has been increasingly used to treat Crohn's disease (CD), its efficacy in preventing postoperative recurrence of CD is still unknown. Here we report a case of a patient with CD localized in the ileum with multiple stenosing lesions and fibrotic tracts. He was previously treated with anti-TNFα agents without disease control. Thus, he underwent laparoscopic ileocecal resection and three ileal strictureplasty surgeries. Ileo-colic resection was performed, and pathology confirmed the presence of a fibrotic stricture. Six months after surgery, magnetic resonance imaging enterography (MRIenterography) documented recurrence of ileal inflammation. Thus, the patient was treated with VDZ according to the induction dosing regimen at weeks 0, 2, 6 and 10, followed by intravenous infusions every 8 weeks, and follow up. After two years of therapy, the patient maintains clinical, endoscopic and radiological remission; Crohn's Disease Activity Index (CDAI) ≤ 110 at all follow ups. To date no anemia, no increase in inflammatory indices, and no abnormal blood tests have been observed. This is a somewhat interesting case because VDZ is used to prevent the postsurgical recurrence of CD in a patient with anti-TNFα treatment failure.
Keywords: Crohn’s disease; Ileocecal resection; Post-surgical recurrence; Vedolizumab
Abbreviations: VDZ: Vedolizumab; MAdCAM-1: Mucosal Addressing Cell Adhesion Molecule-; CD: Crohn's Disease; CDAI: Crohn's Disease Activity Index
Core Tip
Use of Vedolizumab to avoid postoperative recurrence in patients with Crohn’s disease localized in the ileum and with previous anti-TNFα failure.
Introduction
Crohn’s disease (CD) is a chronic inflammatory disease of the gastrointestinal tract characterized by phases of intense activity and of quiescence. The most frequent symptoms are abdominal pain, diarrhea, weight loss, and fatigue [1]. CD affects the entire thickness of the bowel wall, and it can manifest with stenosis, fistulas, abscess, loss of function [2]. To treat these complications, surgery is often required. However, clinical recurrence of CD after surgery is common as it occurs in 30-60% of patients within 3-5 years of index surgery [3,4]. The purpose of therapeutic treatments is to change the natural history of CD and to prevent post-surgical recurrence. Numerous studies show the efficacy of anti-tumor necrosis factor (anti-TNFα) therapy to reduce postoperative recurrence [5], however the effectiveness of VDZ in postoperative management of patients with failure to anti-TNFα, is unknown [6]. VDZ is a monoclonal antibody inhibiting the interaction between the α4β7 integrin and mucosal addressing cell adhesion molecule-1 (MAdCAM-1), resulting in the blocking of lymphocyte homing to the inflamed gut tissue [7].
Case Report
In this case report we describe the history of a 63-year-old Caucasian male. His past medical history included essential hypertension, mild mitral insufficiency, Bosniak type I renal cyst. He was diagnosed with stenosing CD with multiple ileal localizations about 10 years ago. He was treated with anti-TNFα therapy, but both infliximab and adalimumab were disrupted due to allergic reaction and to lack of effectiveness, respectively. In early 2019, the patient was referred to our IBD center for persistent abdominal pain and symptoms of bowel obstruction. Blood tests documented mild anemia (Hb 11,9g/dl), normal leukocytes (WBC 6.82 x10^3/mmc), slight increase in RCP (RCP 2.28mg/dl), normal urine test, and absence of further alterations. We decided to stage the disease by computed tomography enterography (CTenterography) with evidence of multiple ileal stenosing and fibrotic tracts with upstream dilatation and other inflammations (Figure 1). Indication for surgery was given due to previous therapies failure and to the current state of the patient. In July 2019, the patient underwent laparoscopic ileocecal resection and packaging of mechanical anisoperistaltic ileo-ascending latero-lateral anastomosis and three Heineke-Mikulicz ileal strictureplasties. According to the guidelines, six months after surgery we performed colonoscopy and MRIenterography. Colonoscopy documented regular outcomes of endoscopic resection, MRIenterography showed thickened tracts of the neoileum in the preanastomotic area and in the mesogastrium with the presence of subcutaneous fistula. Blood tests did not show significant alterations, however during the physical examination the patient reported pain on palpation of the right iliac fossa and episodes of spontaneous abdominal pain. The patient started VDZ therapy in February 2020 according to the recommended induction regimen at 0, 2, 6 and 10 weeks, without adverse reactions. After one year of therapy, CT enterography (Figure 2) documented improvement in the radiological images, in particular we observed reduction of wall thickening of distal neoileum in the right meso abdomen and reduction in wall thickening of the ileal tract below the umbilicus with return to normal distensibility. Colonoscopy was performed six months after CT enterography and it confirmed the endoscopic remission with stabilized outcomes of ileocecal resection and regular neo ileum (Rutgeerts i0.) The patient has always reported clinical well-being while maintaining the CDAI <110, blood tests did not show significant alterations. After about two years of infusion therapy, VDZ was administered subcutaneously, one every 2 weeks at a dose of 108mg (Figure 3).



Discussion
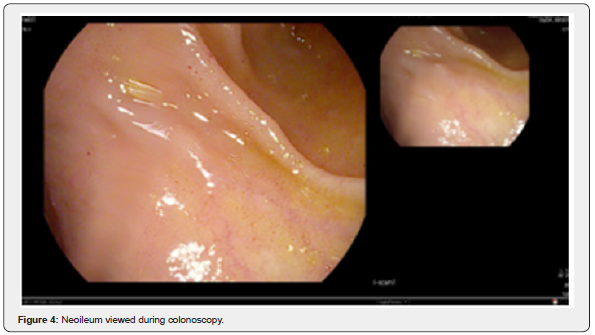
Crohn’s disease is an inflammatory bowel disease causing an uncontrolled inflammatory process in the gastrointestinal tract, with a relapsing and remitting course [1]. It is a complex and life-long condition whose etiology and mechanisms underlying its development are not fully understood [8]. Fortunately, research ongoing and new treatments are increasingly becoming available. Over the past 20 years, anti-TNFα have changed the natural history of these diseases, reducing the long-term requirements of surgery and hospitalization [9-11]. In recent years, new biologics such as VDZ that block leukocyte migration mediated through integrins, have entered clinical practice and increase the chance to obtain better disease control and to improve quality of life [2]. While the use of VDZ in CD is now well established [12], its use in the prevention of post-surgical recurrence still unknown. In the present case report we wanted to document the efficacy of VDZ in a patient operated for CD and not suitable for anti-TNFα to prevent post-operative recurrence. Further large placebo-controlled studies are needed to show the therapeutic benefits and economic implications of these observations (Figure 4).
Author’s Contribution
Antonella Scarcelli designed the work, Annalisa Pasetti and Stefania Maltoni wrote the paper, all authors reviewed and approved the manuscript.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment