Survey of Dental Health Care Workers Regarding Their Knowledge of Viral Liver Disease and Prevention of Its Transmission, Using an Online Questionnaire
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Yumiko Nagao
Abstract
Background: Over three million people in Japan are estimated to be infected with hepatitis viruses. Dentists need to be aware of measures to prevent transmission and have knowledge of extrahepatic manifestations. However, in Japan, there has been little evaluation of dentists’ knowledge of viral hepatitis. We investigated dental care workers for their knowledge of, and countermeasures against, viral hepatitis.
Materials and methods: An anonymous online questionnaire surveying 1,210 members of the Japanese Society of Dental Practice Administration. Interviews were carried out with those who consented. Survey items are attributes, self-management of viral hepatitis, knowledge of liver disease, control of transmission, contacting patients with viral hepatitis, and gathering information on liver diseases.
Results: 153 individuals responded to the questionnaire; 41 had not been immunized against hepatitis B and 61 knew of extrahepatic manifestations. Risk and knowledge deficit scores were significantly higher for workers in dental clinics than those in university settings (p<0.001, p=0.014).
Conclusion: The respondents had insufficient knowledge of viral hepatitis, a low rate of immunization against hepatitis B and may not follow safe medical practice. It is critical that dentists understand the latest information on hepatitis viruses and acquire knowledge and skills related to medical safety and prevention of infection.
Keywords: Dental health care workers, Online questionnaire survey, Hepatitis C virus, Hepatitis B virus, Oral lichen planus, Nosocomial infection control
Abbrevations: OLP: Oral Lichen Planus; HCV: Hepatitis C Virus; HBV: Hepatitis B Virus; SVR: Sustained Virological Response; DAA: Direct-Acting Antivirals
Introduction
It is estimated that more than 3 million people in Japan are infected with hepatitis B virus (HBV) and/or hepatitis C virus (HCV), and the number of liver cancer deaths annually is about 30,000 [1]. About 65% of liver cancer is caused by HCV infection and about 15% is attributable to HBV infection. Recent advances in direct-acting antivirals (DAAs) have been revolutionary in HCV treatment. It is also known that infection with HCV causes damage not only to the liver but also other organs and tissues [2]. Such extrahepatic manifestations include lymphoproliferative, autoimmune, skin-mucosal and metabolic diseases. Lichen planus (LP), Sjögren’s syndrome, and oral cancer have been reported as extrahepatic manifestations in the oral cavity [3-6].
Japan has been in the forefront of countering hepatitis viruses; the introduction of hepatitis virus tests by the Health Promotion Act (conventional old age health law), the so-called ‘turning point examination and examination out of the turning point’ (2002), the implementation of free hepatitis examinations (2007), the establishment of the Hepatitis Information Center (2008), the initiation of the medical expenses subsidy program for interferon treatment (2008), and enforcement of the Basic Act on Hepatitis Measures (2010) are of note. Based on the Basic Act on Hepatitis Measures, the underlying philosophy was established, and the responsibilities of the national government and local governments were clarified. Measures against hepatitis have been promoted comprehensively for the prevention, early detection, and treatment of hepatitis.
Meanwhile, because dental care workers often have contact with bodily fluids, such as the blood and saliva of patients, infection control in dental medical institutions is critical. Measures and knowledge of patients infected with HBV or HCV, the most common infections in our country, are essential for dental health workers. However, dental health workers do not necessarily have sufficient knowledge of hepatitis viruses [7,8]. Patients with viral hepatitis may be subject to discrimination and prejudice from healthcare workers, and it is also a concern that they may not declare their own hepatitis virus infection at a dental clinic [9,10].
To date, there have been few reports in Japan where dentists have been investigated in detail regarding their recognition of viral liver disease. Therefore, in this study, we conducted a survey using the Internet to evaluate the recognition of problems of hepatitis by dentists. If we can clarify the problem using this survey, we can contribute to the dissemination of knowledge of liver diseases to dental health workers.
Methods
Subjects
The subjects are the 1,210 members of the Japanese Society of Dental Practice Administration.
Methods
After all members of the Japanese Society of Dental Practice Administration had been notified, we made the anonymous, questionnaire available online from April 27 to June 30, 2017. We explained the purpose of this study on the first page of the online questionnaire and considered those who responded to have provided consent. After answering the anonymous questionnaire survey, those who agreed to a telephone interview provided their name, address and contact telephone number and submitted a written consent form.
HBV: Hepatitis B Virus; HCV: Hepatitis C Virus
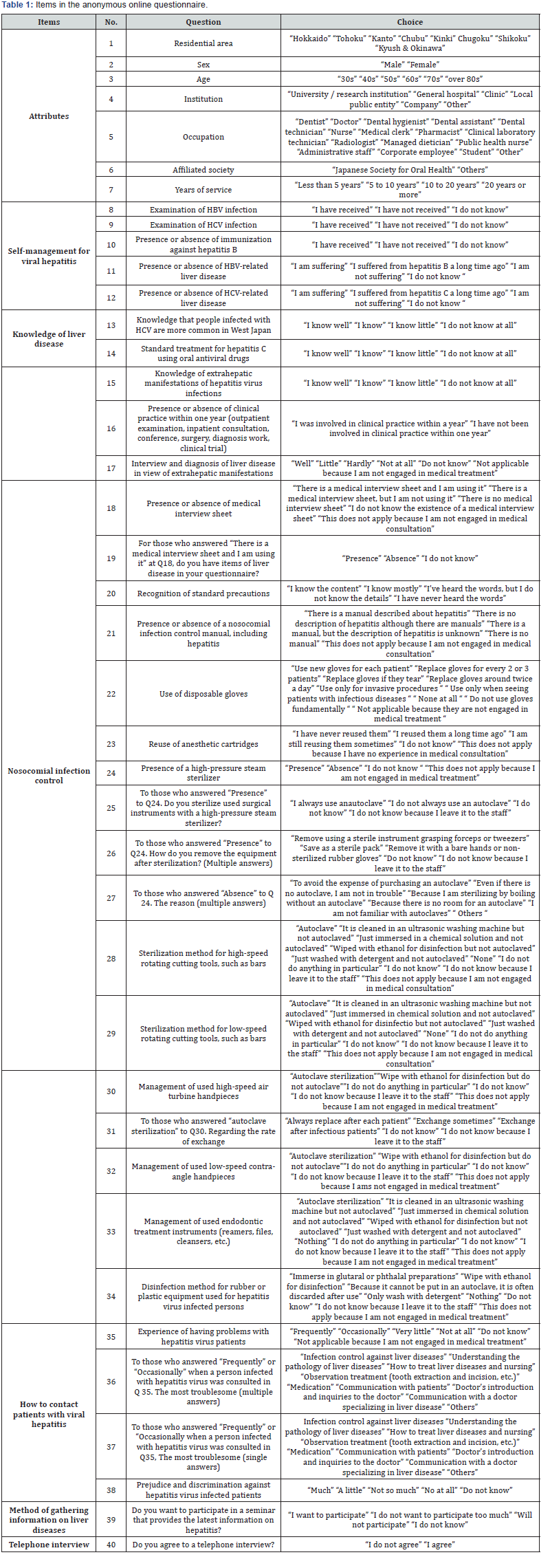
Items in the anonymous, online questionnaire (Table 1):
a) Attributes: Residential area, sex, age, institution, occupation, affiliated society, and years of service
b) Self-management of viral hepatitis: Examination of HBV infection, examination of HCV infection, whether immunized against hepatitis B, presence or absence of HBV-related liver disease, and presence or absence of HCV-related liver disease
c) Knowledge of liver disease: Knowledge that infection with HCV is more common in West Japan, standard treatment for hepatitis C, knowledge of extrahepatic manifestations of infection with hepatitis viruses, and interview and diagnosis of liver disease in view of such extrahepatic manifestations
d) Nosocomial infection control: Presence or absence of medical interview forms, recognition of standard precautions, presence or absence of a nosocomial infection control manual, use of disposable gloves, reuse of anesthetic cartridges, presence of a high-pressure steam sterilizer, and method of sterilization of cutting tools, rotary cutting machines and instruments for root canal treatment after use
e) How to contact patients with viral hepatitis.
f) Method of gathering information on liver diseases.
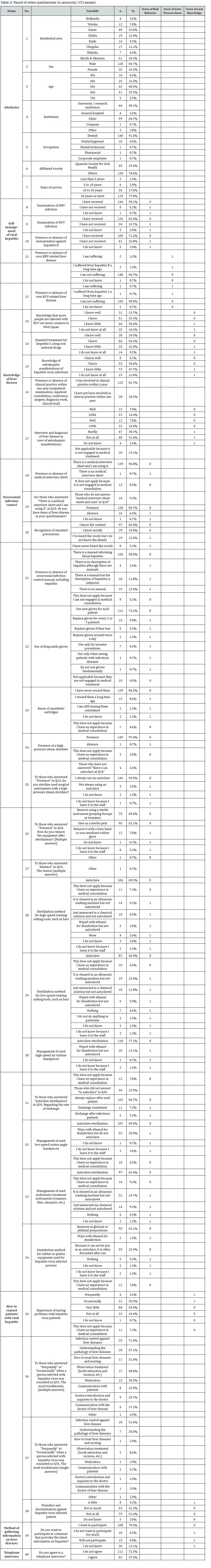
Analysis of items regarding risk behavior and onset of liver disease, and lack of knowledge (Table 2): Among the questionnaire items, risk scores were given to responses that indicated failure to self-manage hepatitis or to take safe hospital infection countermeasures. Risk was scored as 1 point and norisk as zero point. In addition, a responder with liver disease was scored as 1 point and one without liver disease as zero point. A person with no knowledge of liver disease was scored as one point and one with knowledge was scored as zero point. For each subject, the scores were totaled for three items: risk behavior, presence of liver disease and lack of knowledge. A high score indicates a dangerous medical situation.
HBV: Hepatitis B Virus; HCV: Hepatitis C Virus
Items of the telephone interviews: We interviewed by telephone those who provided their documented agreement regarding how to cooperate with medical institutions regarding liver disease patients and how to acquire knowledge of liver disease.
Ethics approval and consent to participate: The study was approved by the Ethics Committee of Saga University (reference number: 28-35 and 29-81) in accordance with the Declaration of Helsinki.
Statistical analysis: Summary statistics are shown as frequencies (proportions) for categorical data and as the mean ± standard deviation (SD) for continuous variables. The differences between groups were evaluated by the 2-sided unpaired Student’s t-test. A p value <0.05 was considered statistically significant. All statistical analyses were performed using R Statistical Software (version 3.4.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
Aggregate online survey
153 subjects (128 men, 25 women) completed the online questionnaires anonymously (Table 2). Individuals aged in their fifties (62, 40.5%) and sixties (51, 33.3%) accounted for about 70% of the total. There were more responses from directors of dental clinics (99 individuals, 64.7%) than university research institutes and workers in general hospitals (50 individuals, 32.7%). Almost all (91.5%) of the respondents were dentists. 77.8% (119 individuals) who had been engaged in medical treatment for more than 20 years.
Of the responders, 144 (94.1%) and 126 (82.4%) had been tested for HBV and HCV infection, respectively, but 41 (26.8%) had not been immunized against hepatitis B. Four (2.6%) and two (1.3%) had HBV-related and HCV-related liver disease, respectively. Only 72 individuals (47.1%) were aware that there are more HCV-infected people in the western part of Japan but 114 (74.5%) recognized that oral antiviral agents (direct acting antivirals, DAAs) are the standard therapeutic agents for hepatitis C. Sixty one (39.9%) knew of the extrahepatic manifestations of hepatitis virus infections and 34 (22.2%) asked questions and carried out medical examinations regarding HCV infection when examining patients with LP.
The answers to the questions regarding measures for infection control were as follows: There were 10 responders (6.5%) who used questionnaires without liver disease items, 126 (82.4%) who understood the contents of the standard precautions, 104 who had produced manuals for infection control measures, 112 (73.2%) who used disposable gloves for each patient, 129 (84.3%) who had never recycled anesthetic cartridges, 143 (93.5%) who sterilized used surgical instruments, 106 (69.3%) who sterilized used high-speed rotating cutting tools such as bars, 87 (56.9%) who sterilized used low-speed rotating cutting tools such as bars, 118 (77.1%) who sterilized used high-speed air turbine handpieces,107 (69.9%) who sterilized used lowspeed contra-angle handpieces, 97 (63.4%) who sterilized used endodontic treatment instruments (reamers, etc.), and 130 (85.0%) who disinfected in a safe way or discarded the instruments used for hepatitis virus-infected patients.
The responses regarding the treatment of patients with liver disease were as follows: Thirty-five (22.9%) had had difficult experiences with hepatitis virus-infected patients, the most serious problem was infection control against liver disease (18/35 individuals, 51.4%), and eight (5.2%) had prejudice and discrimination against hepatitis virus-infected patients. There were 108 responders (70.6%) who wished to participate in seminars providing information on liver diseases.
Analysis of survey items about risk behavior, onset of liver disease, and lack of knowledge
Table 2 shows the scores for risk behavior, onset of liver disease, and lack of knowledge. Table 3 shows average values of the three sets of scores according to residential district, sex, years of service, and institution. The men had a significantly higher risk scores and knowledge deficit scores than the women (p=0.002, p=0.031). Risk scores and knowledge deficit scores were significantly higher for directors of dental clinics than for university workers (p<0.001, p=0.014). Dentists with less than 20 years of experience tended to have a higher knowledge deficit score than those with more than 20 years (p=0.053). There was no significant difference in the relationship between the responder’s residential district and the scores.
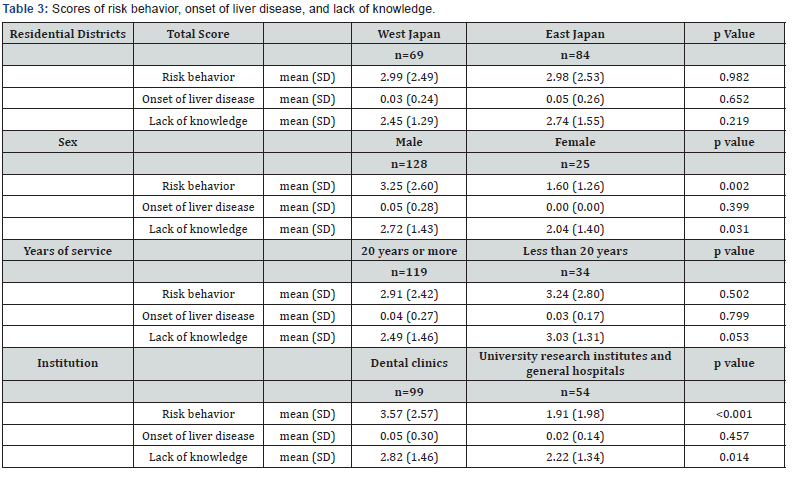
SD: standard deviation
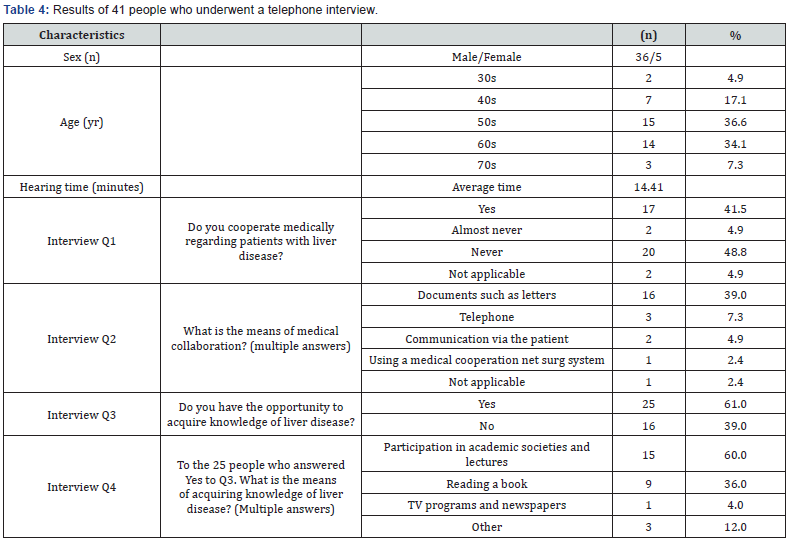
Result of the telephone interviews
All but one of the 42 subjects who agreed to do so participated in a telephone interview (implementation rate 97.6%) (Table 4). The average interview time was 14.41 minutes. Twenty-two interviewees (53.7%) reported “not performing” or “hardly performing” medical cooperation with patients with liver disease. Documents such as letters were the most frequent means of medical cooperation (16 subjects, 39.0%). Twenty-five (61.0%) responded that there were opportunities to acquire knowledge of liver diseases but reported that seminars for dentists about liver diseases were not available.
Discussion
On December 31, 2016, 104,533 dentists were registered in Japan, 80,189 men (76.7%), and 24,344 women (23.3%). (Eighty dentists per 100,000 population.) Regarding the type of facility, 89,166 dentists worked in clinics and 12,385 dentists worked in university research institutes and general hospitals: the proportion of dentists working in clinics is increasing year by year.
In this study, the directors of dental clinics had significantly higher risk scores for infection and deficiency of knowledge of hepatitis viruses and infection control than dental physicians working in university research institutes and general hospitals. This indicates a serious problem in securing medical safety in Japan, where the vast majority of dentists work in clinics. Dentists and dental health care workers are at high risk of infection with HBV and HCV during their daily occupational experiences [11].
Following a survey of 253 Japanese dental students between 2006 and 2007, we reported that their understanding of disinfection and sterilization was insufficient [7]. The introduction of a modified curriculum, with appropriate education of students in these matters, were critical issues. According to a screening study of 141 Japanese dental workers conducted in 2007, fewer than half (48.2%) of the participants had been immunized against hepatitis B [8]. Of 63 immunized individuals, 16 (25.4%) were positive for anti-HBc, indicating past exposure to the virus. The positivity rate of anti-HBc was 85.7% for respondents in their sixties and 100% for those in their seventies; this rate was extremely high for the oldest responders. In routine dental practice, dentists who did not always use disposable gloves accounted for 17% of those who tested positive. Tada et al. surveyed changes in infection control practice reported by dentists in Japan in 2008 and 2011 and factors related to these changes [12]. They reported that the rate of immunization against hepatitis B was 65.4% in 2008 and 67.1% in 2011. Infection control practices significantly associated with the proportion of dentists specializing in oral surgery, the proportion of dentists reporting a willingness to treat HIV and AIDS patients, and the proportion of dentists reporting knowledge on standard precautions. Compliance with effective infection control practices by dentists may be affected by knowledge and education.
We have also reported that 59.8% of HBV and HCV infection with liver disease patients consistently self-declared hepatitis virus infection when undergoing dental treatment [9]. The main reason for not reporting such infections at a dental clinic was because the dentist had not enquired about the possibility of an underlying disease (71.2%).
In the United States, a case of HBV infection related to tooth extraction was reported in 2007 [13]. Nosocomial infection from patient to patient was proved because the HBV nucleotide sequence matched between the patients. In 2013, in the United States, the Centers for Disease Control and Prevention (CDC) issued a report of patient-to-patient transmission of HCV in a dental office [14]. More than 7,000 patients were notified and tested for hepatitis B and hepatitis C viruses and HIV because of unsanitary conditions and improper sterilization of equipment in the office. The Oklahoma State Department of Health reported that 77 people tested positive for hepatitis C, five for hepatitis B and four for HIV.
In Japan, Ogata et al. [15] reported that the major sources of acute hepatitis C virus infection in 2013 were medical procedures and accidental needle sticks. Their study was a retrospective analysis of patients in 12 facilities nationwide who developed acute hepatitis C after 1990. Medical procedures were the most common source of infection, accounting for 32.4% of the 102 patients (33/102). These procedures were as follows: surgery (14 cases), blood transfusion (5), endoscopy (3), intravenous injection (4), invasive procedures (3), dental therapy (3) and dialysis (1).
Mahboobi et al. [16] concluded in their review that dental treatment is a risk factor for acquiring HBV and HCV and that the risk could be eliminated easily using standard precautionary measures.
Based on a revision of the medical law in Japan, general dental clinics were obliged in 2007 to establish medical safety management systems. In June 2014, the Ministry of Health, Labor and Welfare announced a requirement to sterilize the dental handpieces for each patient. In a questionnaire answered by 700 Japanese dental physicians in 2017, the rate of sterilization after replacing used handpieces for each patient was 52%, the rate of exchanging gloves for each patient was 52%, the rate of sterilization after washing used cutting bars was 64% and the ratio of sterilization after washing used root canal treatment devices was 65% [17].
Unfortunately, even in this study of members of the Japanese Society of Dental Practice Administration, the rate of sterilization of instruments was rather low. Despite being at high occupational risk of hepatitis virus infection, only around 70% of the responders had been immunized against hepatitis B The percentage of dentists who treat oral mucosal disease from the viewpoint of extrahepatic manifestations was also small.
Hepatitis C virus is known to cause extrahepatic manifestations such as oral lichen planus (OLP) [6,18]. We performed a genome-wide association study (GWAS) of Japanese HCV-related patients with or without OLP, followed by a replication analysis in an Italian population. It was found that rs884000 in neuropilin- 2 (NRP2), rs538399 on insulin-like growth binding proteins factor 4 (IGFBP4), and rs9461799 (HLA-DR/DQ) were associated with HCV-positive LP [19].
If dentists encourage examination and treatment of hepatitis through dental and medical cooperation, they can identify and treat patients with undiagnosed hepatitis virus infections. We examined retrospectively oral mucosal disease and HCV infection using the medical record information of 90 patients who consulted a general dental clinic [20]. OLP was the most common oral disease. Among 51 patients who could be examined for the presence or absence of HCV infection, the incidence of that infection was 29.4% (15/51). Among the OLP patients who consulted the dental clinic, we identified a new HCV-infected patient and led an untreated HCV-infected patient to a sustained virological response (SVR).
There have been some reports that have assessed stigma and discrimination in relation to HCV infection within the healthcare setting [21]. We performed a survey of the prejudice and discrimination experienced by HCV/HBV-infected individuals from healthcare workers. Prejudice was most prevalent within the dental clinic setting [10].
Conclusion
We conclude that dentists in Japan do not have sufficient knowledge of viral hepatitis, have a low rate of immunization against hepatitis B and do not necessarily carry out safe medical practices, despite having a high risk of infection. We consider that dental care workers need to understand the latest information on hepatitis viruses and to acquire knowledge and skills relatedto medical safety and prevention of infection. It is necessary to treat the oral cavity with a view to cooperative medical treatment between medical departments and dentistry.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment