Clinical Hepatocyte Transplantation_Juniper Publishers
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Toshio Miki
Abstract
A severe shortage of suitable allograft is a long-standing and worldwide problem for the patients who are waiting for organ transplantation. Hepatocyte transplantation has been proposed as an alternative therapeutic approach for liver disease patients to address these urgent and unmet medical needs. The cell replacement approach does not replace the orthotopic liver transplantation (OLT), but rather complement OLT especially for the patients who are not required whole liver replacement such as congenital metabolic disorders. This review article summarizes current knowledge and limitations of clinical hepatocyte transplantation and aims to advance our understanding towards the goal of developing novel cell replacement therapies for the patients who are on the OLT waiting list.
Keywords: Hepatocytes; Congenital metabolic disorders; Cell replacement therapy; Regenerative medicine
Introduction
Hepatocyte transplantation has been proposed as an alternative approach of the orthotropic liver transplantation (OLT). A number of advantages of this cell replacement therapy over the OLT are listed including less invasiveness and cost-effectiveness [1]. The concept of partially replacing damaged or malfunctioned hepatocytes is particularly suitable for the patients who suffer from congenital metabolic disorders and acute liver failure patients who require transient support of their liver function. The keys to the successful hepatocyte transplantation are the indications and the careful evaluation of the eligible recipients, the preconditioning of the recipient’s liver, and the quality of the donor cells. The cell transplantation procedure is technically simple compared to that of OLT. The common interventional technique is required to safely deliver the cells to the liver. Here, we briefly overview the reported clinical cases, suitable target diseases, clinical procedures, limitations, and perspective to overcome the limitations.
History
The basic studies that led to clinical hepatocyte transplantation were initiated in 1970’s. Rodent models with metabolic disorders and acute liver failure models induced by chemicals, partial hepatectomy, or ischemic-reperfusion liver injury were often used to demonstrate improvements of damaged liver functions by injecting autologous liver cells [2]. These pre-clinical studies indicated that the allergenic liver cell transplantation had a potential to correct various metabolic defects. The earliest published reports of pre- clinical hepatocyte transplantations were performed in 1976 by a group led by Najarian using UDP-glucuronyl-transferase-deficient rats, the Gunn rat [3]. About a decade later, Mito tested an idea to utilize the spleen as an ectopic liver by transplanting hepatocytes into the spleen with rodent and dog models [4].
The first attempted human hepatocyte transplantation was performed in 1992 by the same group in Japan [5]. The safety of hepatocyte splenic arterial infusion and the therapeutic efficiency were confirmed by Strom [6] with chronic end- stage liver disease patients. They demonstrated that transplanted human hepatocytes were viable in splenic nidation and showed typical hepatic cord structures. Three of five treated patients fully recovered and successfully received OLT. Since then, more than 100 clinical hepatocyte transplantations were reported [7-9]. Over the last two decades, more than 15 institutes around world sporadically conducted clinical hepatocyte transplantation, and currently, at least 7 groups are active [6]. However, despite these successes of the clinical studies, hepatocyte transplantation has remained experimental due to the limited supply of donor liver tissue for hepatocyte isolation. Conducting a large-scale randomized clinical trial has been prohibited by the limited supply of sufficient and consistent quality of human hepatocytes.
Indications
Orthotropic liver transplantation (OLT) is a significantly efficient treatment to improve the prognosis in patients with fulminant hepatic failure, end-stage liver disease, and metabolic liver diseases. In theory, if we can replace 100% of damaged patient’s hepatocytes, hepatocyte transplantation can provide similar therapeutic efficacy in most of these diseases. Therefore, the indication of hepatocyte transplantation depends on how much replacement is required to alleviate disease symptoms and how much donor cells can functionally engraft in the patient’s liver. In addition, the indications will depend on the risk-benefit balance. Based on this logic, the disease conditions that inhibit donor hepatocyte engraftments such as cirrhotic liver and acute hepatitis will not be suitable.
On the other hand, congenital metabolic disorders (CMDs) will benefit from hepatocyte transplantation. In general, metabolic disease patients require only partial replacement of hepatocytes to compensate for the missing enzyme function. The required compensation level may vary by case and by disease. Careful assessments of the impaired enzyme functions will be required to determine the indication of hepatocyte transplantation. Approximately 1 in 1,500 children is born with a CMD. Many of these critical inborn errors of metabolic or synthetic processes involve principally the liver. Current therapy for CMDs consists of life -long dietary restriction with or without supplementation of amino acids. For example, an infusion of normal hepatocytes that is equivalent to 5% of the parenchymal mass achieved a medium-term reduction in serum bilirubin in a patient with Crigler-Najjar syndrome [10]. An ornithine transcarbamylase deficient child who received 1.9x109 hepatocytes had normalization of plasma ammonia and glutamine levels on a normal diet without phenylbutyrate/ phenylacetate therapy. These cases clearly demonstrate CMDs can be effectively treated via cell replacement therapy.
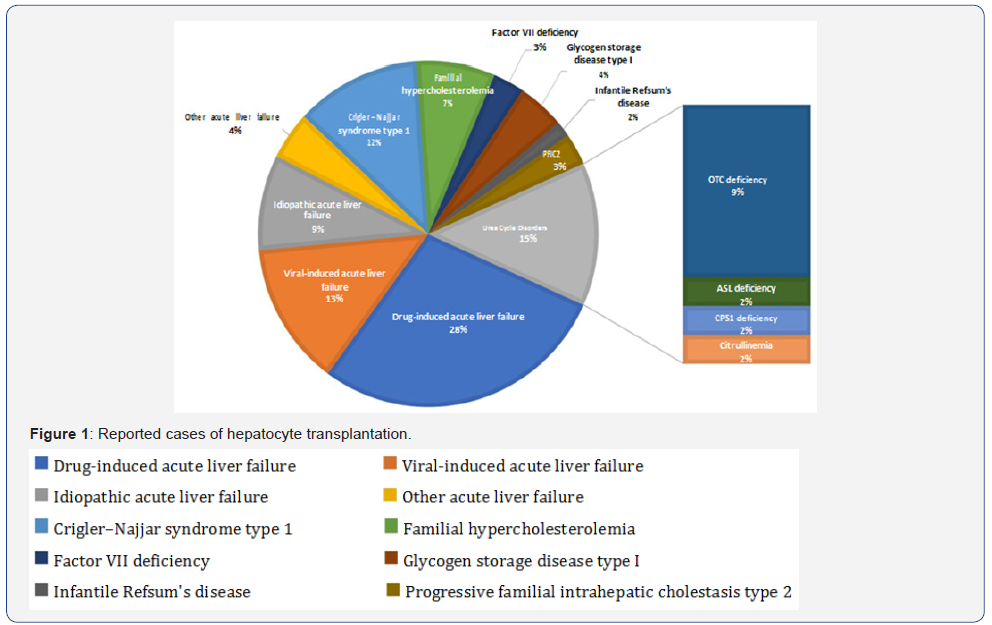
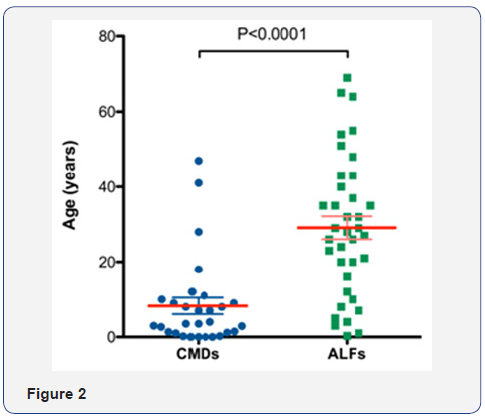
Acute liver failures will also benefit from the cell replacement strategy. Although the liver is still in the active inflammation status, injecting hepatocytes into the spleen may support the patients’ hepatic function temporarily until the own liver recovers or until the OLT become available. A total of 68 reported clinical hepatocyte transplantation cases can be categorized in these two groups, CMD and ALF (Figure 1). Due to the epidemiologic nature, the patients’ ages are significantly distinguished (Figure 2). In most of CMD cases except a case with Progressive familial intrahepatic cholestasis type 2, the therapeutic efficacies were partial but satisfactory. Recipients with some conditions may preclude a successful transplant. Such contraindications may include metastatic cancer outside of the liver, active drug or alcohol abuse, and active systemic infections. However, unlike OLT which is a major surgery with a high incidence of complications, the list of contraindications is shorter for hepatocyte transplantation.
Overview of Clinical Practices
Cell sources
The source of primary human hepatocyte is the livers unused for OLT. In result of increasing usage of marginal-suboptimal donor organs with the extended donor criteria (EDC), the availability of organs for cell isolation has diminished. The quality of available donor organ for cell isolation is frequently poor. The degree of steatosis affects the yield, viability, and function [11]. Hepatocytes can be obtained from livers removed from OLT recipients with congenital metabolic disorders. These hepatocytes can be used to treat different types of congenital metabolic disorders [12]. The donor criteria can be extended to advanced-age donors and non-heart-beating donors [13]. However, the cell quality is highly variable. Therefore, these cell sources are not reliable and insufficient to overcome the primary human hepatocyte shortage problem. Hepatocyte Isolation requires well established a unique enzymatic digestion technique. The standard protocol was established based on Seglen’s two-step collagenase perfusion technique for rat hepatocytes isolation. The protocol was slightly modified for human hepatocyte isolation [14-16]. Hepatocytes should be transplanted as soon as possible, preferably within 24hrs of isolation, as the hepatic function deteriorates when kept at 4 ˚C.
Cell dose and route of administration
Although 100% replacement of disease hepatocytes with healthy functional hepatocytes is ideal, the practical goal of replacement ratio will be 10-15%, which may improve enzyme functions to the mild phenotype from the most of severe type congenital metabolic disorders [17-22]. It is assumed that 2×108 cells per kg of body weight may be the upper limit of hepatocytes that can be safely infused during transplantation. The currently proposed optimized dose is 30-100×106 cells/kg of body weight at an infusion rate of 5-10ml/kg per hour, and a concentration of 1-10×106 cells/ml [23]. To achieve the estimated number of cell transplantation, therefore, multiple infusions are necessary with certain interval periods [24].
Cell transplantation performed to target either liver or spleen. Although cell engraftment in the liver is physiological, spleen could be a good alternative destination in case the recipient’s liver suffer from severe fibrosis (cirrhosis). The route of administration must be intraportal injection regardless directly inject into the intra hepatic portal vein, inferior mesenteric vein, umbilical vein, or via spleen. Systemically injected cells will be trapped in the lung and may cause the pulmonary thromboembolism. On the other hand, cells injected into portal vein do not pass through the liver [25]. Although the mechanism of cell integration in the recipient’s hepatic lobule structure is not well studied, it is speculated that the intraportal infusion causes cell embolism at the intra hepatic portal capillary and increase the portal pressure. The portal hypertension and mechanical expansion stimulate intercellular signaling exchange between the non parenchymal cells which increase the vascular permeability [26,27].
Recipient Liver Preconditioning Treatments
Preconditioning treatments are common strategies used in preclinical studies to enhance engraftment and proliferation of donor cells [28]. The aims of the preconditioning treatments can be classified into four categories:
(1) Decrease recipient’s immune reaction.
(2) Disrupt the native liver structure.
(3) Stimulate liver regeneration signalings and
(4) Supress the native hepatocyte proliferation.
The most common treatment is a partial hepatectomy combined with radiation or drugs, such as retro sine [29,30]. Although many of these strategies are not clinically acceptable, Fox [10] demonstrated a significant increase of cell engraftment with partial radiation in clinical hepatocyte transplantation [31]. Irradiation approach may serve all above four aims [32,33].
(1) The irradiation inhibits the phagocytic activity of Kupffer cells.
(2) Transiently disrupt the sinusoidal endothelial barrier.
(3) Induce apoptosis of native hepatocytes to stimulate liver regeneration and
(4) Inhibit native hepatocyte proliferation.
In addition, these effects can be controlled by optimizing the radiation dose. A total dose of 10Gy for patients greater than 3 years of age, and 5Gy for patients less than that age was used in the clinical trial [31]. The donor cells injected into the portal vein were guided to the irradiated right lobe by the left branch occlusion. One of the advantages of hepatocyte transplantation is the native liver serves as a back-up to the therapy. Unlike OLT, the patient’s condition only returns to the pre-transplantation state in case of cellular graft failure. A major concern of this preconditioning treatment is losing this advantage. The eligible recipients must be evaluated carefully.
Limitations/Obstacles and Future direction
There are several obstacles to provide this promising therapy to the patients as an option of standard therapies. Shortage of donor organs limits the availability of livers for hepatocyte isolation. In an endeavour to increase the opportunity to obtain primary human hepatocyte, the researchers extended the donor criteria to advanced -age donors and non-heart-beating donors. Fetal hepatocytes or immortalized hepatocytes were also considered as alternative cells [34]. However, none of them could resolve the problem. Recent advancements in stem cell research have demonstrated that hepatocyte -like cells can be derived from human stem cells.
Pluripotent stem cells such as embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) possess tremendous differentiation potentials, however, the developmental capability is a double-edged sword, associated with the risk of tumorigenicity [35]. It is almost impossible to guaranty the safety of injecting over two billion ESC or iPSC-derived hepatocytes with current technology. Other stem cells such as mesenchymal stem cells also proposed that they possess the hepatic differentiation capability. However, efficiency is still open to debate. One of the placental stem cells, human amnion epithelial cells (hAEC) has been getting attention as an alternative for hepatocyte transplantation [36,37]. hAECs possess multi- lineage differentiation potential including the ability to differentiate towards the hepatic lineage, which allows them to express the desired enzymatic functions [38].
Unlike other components of the placenta, the human amniotic epithelium is derived from pluripotent epiblasts [39-41]. Studies showed that the embryonic stem cell surface markers TRA1-60, TRA1-81, SSEA3, and SSEA4 are positive on most of the fetal amniotic epithelium and some of these stem cell marker positive cells are retained in term placental amniotic epithelium [40]. Primary hAECs respond to exogenous stimuli in vitro and can be induced towards specific differentiation. These morphological and transcriptional profile changes demonstrate the developmental plasticity of the hAECs. Under appropriate culture conditions, hAECs exhibit the capability of differentiating into endoderm lineage tissues including hepatocytes in vitro and in vivo.
Transcriptional analysis of hAECs transplanted SCID/ Beige mouse livers indicate that transplanted hAECs terminally differentiated into mature hepatocytes in mouse liver and expressed functional marker genes including cytochrome P450 genes at equivalent levels to human primary hepatocytes [42]. Several preclinical studies have demonstrated that the hAECderived hepatic cells acquire the desired enzyme function for the treatment of congenital metabolic disorders using disease model animals [43,44]. Other preclinical studies also demonstrated significant therapeutic properties of hAEC for cirrhosis [45].
Importantly, upon transplantation into the livers of mice, undifferentiated hAECs have been shown to engraft, display hepatocyte-like morphology, and express various hepatic enzymes without tumorigenicity. The lack of direct monitoring/ tracking technology after cell transplantation is another obstacle that prevents to make the cell therapy as one of the standard therapies [46]. The biochemical elevations of serum concentrations of aspartate transaminase (AST) and alanine transaminase (ALT) are the markers of liver rejection post OLT, as well as the histological signature of inflammatory cell infiltration in the graft. However, relatively less number of donor cells in case of hepatocyte transplantation limit to determine cell rejection with these assays.
Molecular biological approaches such as detecting Y chromosome sequences with qRT-PCR may be able to demonstrate the presence of donor cells, however, it will not indicate the cell viability. If the target enzyme function is restored or improved, that could be an indirect evidence of cell engraftment. However, these parameters may not be sensitive enough to control immune suppression in a practical manner. Development of novel methods to label cells will be required with a detection/tracking technology with single cell level high resolution. Novel biomarkers that correspond to the rejection will be helpful to optimize the immune suppression regimen [47,48]. It is critical to monitor the status of transplanted cells in order to optimize and design immune suppression regimen for each patient [49].
Currently similar immune suppression regimen used for OLT or islet transplantation is used for hepatocyte transplantation however, it could be reduced because of the immune privileged nature of the hepatocytes [50]. In summary, clinical hepatocyte transplantation studies have clearly demonstrated that this therapy is a suitable treatment for patients with CMDs. However, there are some obstacles to provide this promising therapy to the patients as an option of standard therapies. The obstacles are the insufficient supply of donor cells, the lack of direct monitoring/tracking technology after cell transplantation, which subsequently causes the difficulty to optimize immune suppression protocols. Further studies on stem cell-derived hepatic cells and finding novel biomarkers are required to translate the hepatocyte transplantation into clinic.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment