Huge Juvenile Polyps of the Stomach: A Case Report_Juniper Publishers
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Tsutomu Nishida
Abstract
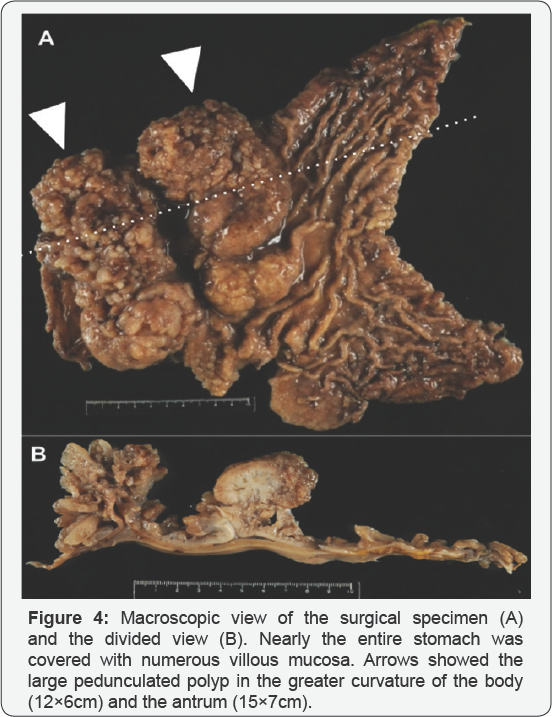
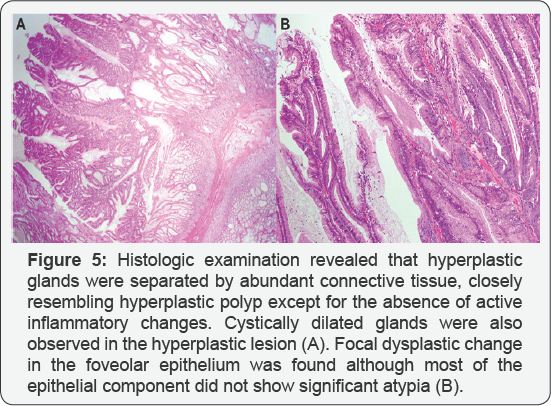
A 46-year-old man with no familial history of polyposis presented with diARGHhea for 2 months. Laboratory data showed anemia, and mild hypoproteinemia. Computed tomography shows two huge tumors in the stomach. Esophagogastroduodenoscopy showed two huge polyps and giant folds covering nodular mucosa in the stomach. Chromoendoscopy with indigo carmine showed that polyps with finger-like villous mucosa were partially reddish and had much mucin. All biopsy specimens from the polyps and randomly collected gastric mucosa indicated hyperplastic changes. Colonoscopy showed several sporadic adenomatous polyps. We diagnosed the patient with huge gastric hyperplastic polys causing protein losing and anemia and sporadic colonic adenomatous polyps. We performed gastrectomy. Immediately after surgery, he stopped diARGHhea and recovered hemoglobin and serum protein levels. Histological examinations revealed that hyperplastic glands with cystically dilated glands were separated by abundant connective tissue. Focal dysplastic change in the foveolar epithelium was found. Finally, we diagnosed juvenile polyps with focal dysplasia limited to the stomach.
Keywords: Gastric juvenile polyp; Gastric polyp; Protein losing gastroenteropathy
Introduction
Juvenile polyposis is a syndrome presented with multiple hamartomatous polyps and generally defined as the occurrence of dozens or hundreds of juvenile polyps of the gastrointestinal tract. Juvenile polyps may develop sporadically or may be associated with the familial juvenile polyposis syndrome (JPS). Patients with JPS are at increased for colorectal and gastric cancer [1].
Juvenile polyposis are divided into three categories;
- Juvenile polyposis of infancy
- Juvenile polyposis coli, and
- Generalized juvenile polyposis [2].
Watanabe et al. [3] first reported a case of juvenile polyposis of the stomach in 1979. Since after, it was proposed as the fourth category of juvenile polyposis [4]. Juvenile polyposis of the stomach is, however, difficult to diagnose because of rare phenotype and difficulty of differential diagnosis between juvenile polyp and foveolar hyperplastic polyp histologically by biopsy specimens. We herein report a case of juvenile polyposis of the stomach.
Case Report
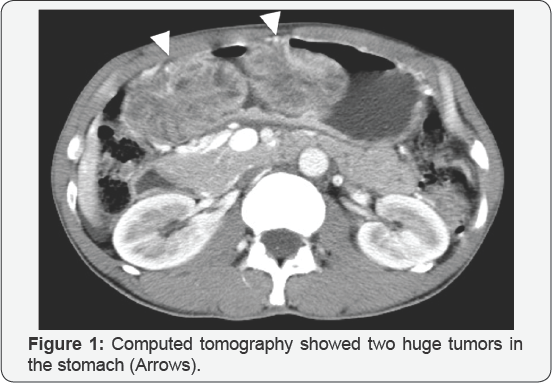

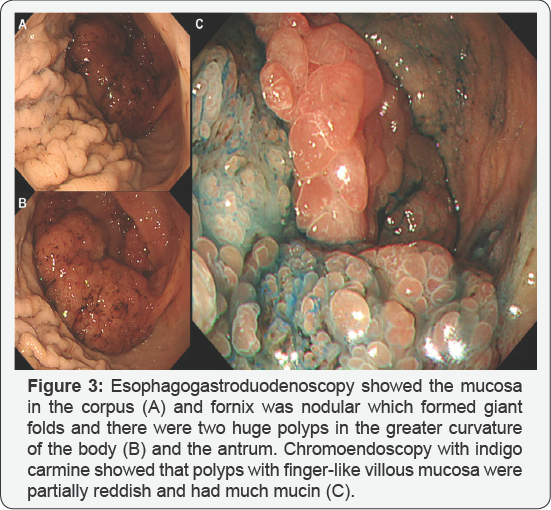
A 46-year-old man with no familial history of polyposis presented with diARGHhea for 2 months. Laboratory data showed anemia (hemoglobin 7.1g/dL), mild hypoproteinemia (total protein 5.4g/dL, albumin 3.0g/dL) and negative for anti-W. pylori anti-body. He presented with no abnormality of the ectodermal- derived tissues, including skin or nail. Computed tomography showed two huge tumors in the stomach (Figure 1). Double-contrast barium study showed numerous gastric polyps (Figure 2). Esophagogastroduodenoscopy showed edematous giant folds covering nodular mucosa in the gastric body (Figure 3A) and two huge polyps in the greater curvature of the body (Figure 3B) and the antrum. Chromoendoscopy with indigo carmine showed that edematous polyps with of finger-like, different sized, villous appearances were partially reddish and had much mucin (Figure 3C). All biopsy specimens from the polyps and randomly collected gastric mucosa indicated hyperplastic changes and no evidence of dysplasia or carcinoma was present. Colonoscopy showed several sporadic adenomatous polyps. We diagnosed him with huge gastric hyperplastic polys causing protein losing and anemia and sporadic colonic adenomatous polyps. We performed distal gastrectomy and colon polypectomy Resected specimens showed that nearly the entire stomach was covered with numerous villous mucosa and there were two large pedunculated polyps in the greater curvature of the body and the antrum (Figure 4). Histological examinations revealed that hyperplastic glands with cystically dilated glands were separated by abundant connective tissue. Focal dysplastic change in the foveolar epithelium was found (Figure 5A & 5B). Histology of colon polyps were adenomaouts polyps including mucosal adenocarcinoma. Immediately after surgery in a month, he stopped diARGHhea and recovered anemia and serum protein levels. After that, we examined the small intestine by barium studies but no polypoid lessons were detected. Finally, we diagnosed juvenile polyposis of the stomach with focal dysplasia.
Nine months later, surveillance EGD showed nodular mucosa grew into polypoid lesions with remarkable reddens in the remnant stomach. We could not deny those polypoid lesions had dysplasia or neoplasms and then we performed total gastrectomy of the remnant stomach. There was no neoplastic lesion in the remnant stomach. After 2 years after second surgery, no juvenile polyposis developed in the small intestine and the colon by surveillance colonoscopy and barium study.
Discussion
Juvenile polyps may develop sporadically or may be associated with the familial JPS that are generally defined as the occurrence of dozens or hundreds of hamartomatous polyps in the gastrointestinal tract, specifically in the stomach, small intestine, colon, and rectum.
The diagnosis of JPS can be clinically made if any following conditions are present;
- More than five colorectal juvenile polyps,
- Multiple juvenile polyps throughout the gastrointestinal tract, or
- One or more juvenile polyps with a family history of juvenile polyps.
Juvenile polyps develop from infancy within the first few years of life through adulthood and are accompanied by hypoproteinemia, protein-losing enteropathy, diARGHhea, anemia, and edema. JPS is an autosomal dominant condition reported to be associated with germline mutation in the SMAD4 or bone morphogenetic protein receptor type-1A (BMPR1A) genes [5,6], which are related to the transforming growth factor-beta (TGF- beta) signaling pathway [7]. When BMPR1A is activated through phosphorylation, it phosphorylates SMAD family proteins [5]. Mutation of those genes are observed in about 60% of patients with JPS. About 25% of patients have de novo mutations.
Sporadic juvenile polyps of the colon are considered benign and occur in up to 2% of children under the age of 10 years [8]. Most of them are solitary and do not require further follow-up [9]. In contrast, patients with JPS who range from 9% to 50% can develop malignant transformation [1,7,10]. In the present case, it was difficult to diagnose this case as JPS prior to the surgery because all biopsy specimens indicated hyperplastic changes without dysplasia and he had no family history of juvenile polyps. We preoperatively diagnosed gastropathy due to huge hyperplasic polyps. Therefore, we performed distal gastrectomy because of two huge polyps causing anemia and hypoproteinemia. Consequently, immediately after surgery, he stopped diARGHhea and recovered hemoglobin and serum protein levels although it remained potential malignancy in the remnant stomach. Reviewing retrospectively, it was endoscopically difficult to evaluate coexistence of dysplasia because of a lot of polyps with much mucin but endoscopic findings showed specific for juvenile polyps. Endoscopically, juvenile polyps are soft, edematous, reddish, and lustrous and sometimes with rich mucin and vary in size from a few millimeters to over 5cm. Histopathology features of juvenile polyps show a normal epithelium with a dense stroma, an inflammatory infiltrate, and a smooth surface with dilated, mucus-filled cystic glands in the lamina propria. It seems difficult to distinguish between juvenile polyp and foveolar hyperplastic polyp histologically by biopsy specimens. Therefore, we think endoscopic findings of JPS, especially juvenile polyposis of the stomach, are important for considering differential diagnosis because of the possibility of bearing malignancy. In addition, polyps in this case were too large and negative for H. pylori infection considering foveolar hyperplastic polyps.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php




Comments
Post a Comment