Clear Cell Sarcoma of Ileum in an Elderly Male: A Rare Case with Review of Literature_Juniper Publishers
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Sanjay Kumar Yadav
Abstract
Clear cell sarcoma, a very rare type of soft tissue sarcoma is mostly seen in extremities of young adults. Gastrointestinal tract is a very rare anatomical location for clear cell sarcoma. Only isolated case reports have been published. We are reporting a 65 years old male patient who presented with history of bleeding per rectum and features of sub-acute intestinal obstruction. The patient underwent contrast enhanced abdominal computerized tomography (CT), which showed circumferential wall thickening extending about 5 cm in length, causing concentric nARGHowing of the lumen of ileum. At laparotomy, mass was resected out from distal ileum and end to end ileo-ileal anastomosis was done. Final histopathological report suggested it to be a clear cell sarcoma. After 8 months of surgery, patient is disease free and doing well.
Keywords: Soft tissue sarcoma; clear cell sarcoma; Ileum
Introduction
Clear cell sarcoma (CCS) is a rare malignant tumor that was described first by Enzinger [1]. Owing to it's clinical, pathological and morphological similarities with melanoma, it is also termed as soft tissue melanoma. Deep soft tissues of the lower extremities close to the tendon, fascia, or aponeuroses are most common sites for CCS [2]. This aggressive malignancy is preferentially seen in adolescents and young adults and is associated with a high propensity of local recurrence, regional lymph node metastases, and distant metastases [1,2]. Primary gastrointestinal tract involvement with CCS is extremely rare. Thus there is lack of information regarding optimal management of GIT CCS and evidence based treatment protocol is still elusive. We are reporting an ileal CCS with 7 months follow up.
Case Presentation
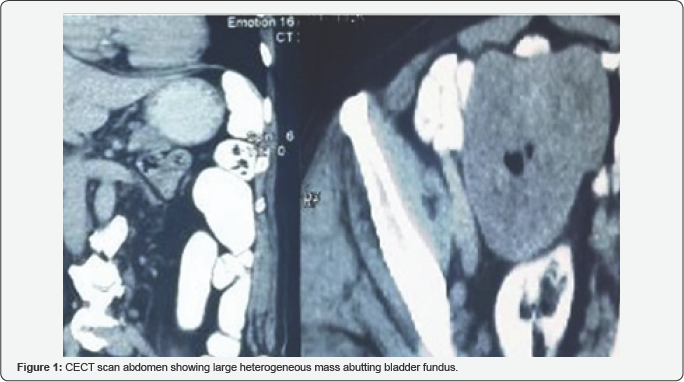
A 65-years-old male patient presented to our emergency department with complaints of intermittent colicky pain, bleeding per rectum and intermittent abdominal distension for five months. There was no history of vomiting, jaundice or tuberculosis. On physical examination, patient had pallor and a firm, non-tender, mobile lump was palpable in right iliac fossa. Digital rectal and proctoscopic examination did not reveal any ano-rectal pathology. Ultrasonography of whole abdomen showed a hypo-echoic space occupying lesion. Contrast enhanced computed tomography (CECT) of abdomen showed fairly large (11x8.5x7 cm approximately), lobulated and heterogeneously enhancing space occupying lesion inferiorly abutting the bladder fundus. No retroperitoneal mass was present (Figure 1). USG guided fine needle aspiration cytology suggested low grade soft tissue sarcoma. Apart from normocytic normochromic anaemia (Hb% 8.5gm/dl), other routine biochemical tests were within normal range. Chest X Ray was normal.
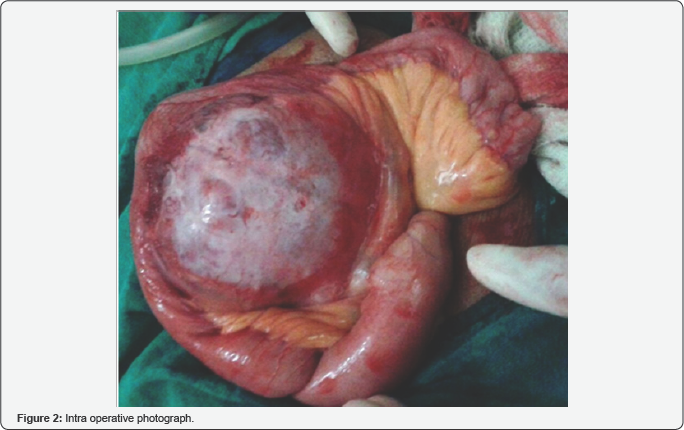
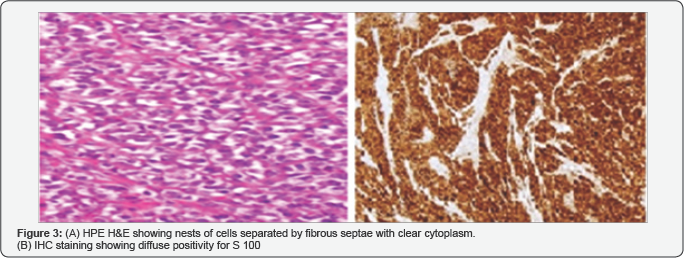
The patient underwent elective midline laparotomy and a nodular mass was recognized at the level of the ileum, 10 cm proximal to ileo-colic junction (Figure 2). Excision of the mass along with partial excision of ileum with end-to-end ileo-ileal anastomosis was performed. Mass was sent for histopathogical examination. Patient was discharged on seventh post-operative day. He is in regular follow up and doing well. HPE showed tumor consisting of fascicles of small rounded cells separated by fibrous septa. Individual cells had abundant clear cytoplasm and vesicular nuclei with prominent nucleoli. Tumor was diffusely infiltrating the small bowel wall. The tumor were strongly positive for S100 protein, with focal weak staining for epithelial membrane antigen (EMA), CD56, and neurone-specific enolase (NSE). It was negative for all other markers: CD117, DOG1, desmin, SMA, h-caldesmon, HMB45, MelanA, CD34, AE1/AE3, Cam 5.2, chromogranin, synaptophysin, neurofilament, HCG, and AFP (Figure 3).
Discussion
Tumors arising from soft tissues are uncommon in ADULTS, accounting for about 01% of all adult malignancies. Soft tissue sarcomas (STS) originating from the striated muscles are called rhabdomyosarcomas (RMS) and remaining group consists of a heterogenous collection of subtypes referred to as nonrhabdomyosarcoma soft tissue sarcomas (NRSTS). CCS is extremely rare type of NRSTS. Enzinger [1] described CCS as a primary mailgnancy of young adults, predominantly involving distal extremities, and presenting as a slowly enlarging mass that has been evident for several months or even years. The principal sites of CCS are the extremities, especially the region of the foot and ankle. The head, neck, and trunk regions are only rarely involved. Involvment of GIT is extremely rare event.
The main characteristic of CCS is its morphological, immunohistochemical and ultrastructural similarity to malignant melanoma [2]. But CCS lacks BRAF mutation and is characterized by a recurrent chromosomal translocation t (12;22), which results in fusion of the EWS gene on 22q with the ATF1 gene on 12q [3]. The presentation of disease consists of intestinal obstruction, anemia or gastrointestinal bleeding [4]. Confirmation of diagnosis usually requires excision of mass followed by HPE and IHC staining. Usually the tumor consists of nests of small rounded cells which are separated by fibrous septa. They have abundant clear or eosinophilic cytoplasm and vesicular nuclei with prominent nucleoli. A confirmation of diagnosis is obtained by immunohistochemistry with a diffuse or focal positivity for S-100 protein and melanocyte-associated antigen HMB-45, positivity for neuron-specific enolase (NSE).
Unlike most soft tissue sarcomas, CCS often metastasizes to regional lymph nodes [1,2]. Distant metastasis is commonly to liver. Complete excision of the primary tumors appears to be the optimal approach to treatment [5]. Various chemotherapeutic regimens for musculoskeletal sarcomas are being used, including actinomycin, Adriblastina, cyclophosphamide, carboplatine, cisplatine; dacarbazine, etoposide, fotemustine; iosfamide, interleukin 2, ifosfamide (3 g/m2) + dactinomycin (1,5mg/m2) + vincristine (1,5 mg/m2); MAID: doxorubicine (15mg/m2) + dacarbazine (250 mg/m2/j) + ifosfamide (2-2,85 g/m2/j), vincristine; VACA: cyclophosphamide (1,2 g/m2) + doxorubicine (30 mg/m2) + dactinomycin (0,5 mg/m2) + vincristine 1,5 mg/ m2; intrferon and taxol [7,8]. But there is no consensus on adjuvant chemotherapy or radiotherapy for GI CCS. Our patient did not receive any adjuvant therapy. A total of 21 GI CCS cases have been reported in the literature, more often arising in the ileum (10 cases) and less commonly in other sites, such as the jejunum (six cases) the duodenum (one case), the stomach (one case) and the colon (three cases) [4,6]. Ours is most probably only 11th case of ileal CCS in english language literature.
Conclusion
To conclude about CCS is extremely difficult because of it's rarity. GI CCS is an aggressive malignancy with poor prognosis. Complete resection with negative margin remains only hope for cure
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php




Comments
Post a Comment