Systematic Review: Laparoscopic Gastrectomy in Locally Advanced Gastric Cancer: Is It Viable?_Juniper Publishers
Authored by Luiz Ronaldo Alberti
Abstract
Introduction: Gastric cancer is one of the
most important pathologies of the digestive tract, representing the
fifth most common cause of cancer, with the adenocarcinoma being the
main histological type. Standard approach for the treatment of the
gastric tumors is surgical resection, performed laparotomically or
laparoscopically. In the past years, the minimally invasive procedure
had a significant improvement making the laparoscopy progressively
viable, mostly for the initial early staged tumors.
Objective: This systematic review aims to
determine the efficiency of the laparoscopic approach on the treatment
of locally advanced gastric cancer.
Methodology: The present study is a systematic review of eight systematic reviews published in the past 5 years.
Discussion: According to the publications
analyzed, the only parameter in which conventional gastrectomy was
superior to laparoscopic gastrectomy was surgical length. Many authors
justify this difference by saying that the minimally invasive procedure
has a higher complexity of performance of the gastrointestinal transit
reconstruction, as well as the more complex lymphadenectomy. It is also
take into account the preparing of materials and laparoscopic
instruments, the decrease of tactical sensation and the different levels
of expertise of the surgeons performing the procedure. Bleeding, length
of hospitalization, pain and complication rates was all smaller in the
laparoscopic approach.
Conclusion: Based on all the analyzed reviews,
laparoscopic gastrectomy proved to be as viable as the conventional
technique when opted for approach of a gastric adenocarcinoma,
presenting, in the majority of parameters, better results than of open
surgery. Nevertheless, some considerations are still necessary.
Introduction
The gastric cancer is one of the most important
pathologies of the digestive tract, representing the fifth most common
cause of cancer, with the adenocarcinoma being the main histological
type [1].
It is staged according to the 7th edition of the American Joint
Committee on Cancer (AJCC) staging manual for gastric cancer, in which
it was determined that the early stage (T1) is when the tumor remains
confined to the sub mucous tissue, with or without lymph node
metastasis, and the advanced stage being the one with invasion of
submucous tissues [2].
According to the Brazilian Consensus of Gastric Cancer, issued in 2013
and following AJCC staging parameters, the locally invasive gastric
cancer is the one classified by the TNM system as T4N0- 2M0, meaning
that there is invasion of visceral peritoneum (serosa), with lymph node
metastasis up to 6 regional lymph nodes, without metastatic disease (M0)
[3,4]. Being the abovementioned parameters the ones used to assess the level of invasion of gastric tumors in this study.
According AJCC's 7th edition, the survival rates
observed above 5 years, according to each stage, are: T1-98%; T2-75,8%;
T3-48,9%; T4-25% [4].
Due to this statistics, it is advisable thotrat the patient as soon as
possible, having a higher possibility of live free of disease, and being
less surgically aggressive in order to improve post operative status.
The standard approach for the treatment of the
gastric tumors is surgical resection, performed laparotomically or
laparoscopically. The laparotomic gastrectomy - also called open or
conventional gastrectomy (CG)-is made by a midline incision or by the
Chevron incision (also known as bilateral subcostal incision or double
Kocher incision). For the laparoscopic gastrectomy (LG), two different
approaches can be used, depending on the option for the reconstruction
of the intestinal transit. The laparoscopically assisted gastrectomy
(LAG) uses a 5cm epigastric mini-laparotomy (besides the laparoscopic
trocar placement) in order to perform the anastomosis outside de
abdominal cavity. In other hand, the totally laparoscopic technique for
gastrectomy (TLG) uses only the trocar placement as approach due to the
intrabdominal anastomosis [1,4].
The first reported laparoscopic surgery for gastric
cancer was made in 1994 by Kitano, who performed a LAG with
lymphadenectomy for an early staged gastric tumor [5].
In the past years, the minimally invasive procedure
had a significant improvement making the laparoscopy progressively
viable, mostly for the initial early staged tumors. The efficiency and
safety of the laparoscopic approach in tumors with higher staging, such
as the locally invasive, is under discussion and has not been
established yet.
Therefore, this systematic review aims to determine
the efficiency of the laparoscopic approach on the treatment of locally
advanced gastric cancer
Methodology
The present study is a systematic review of eight
systematic reviews published in the past 5 years. The databases PubMED,
SciELO and LILACS were used for the research of the following keywords:
"laparoscopic gastrectomy locally gastric cancer”; "laparoscopic
gastrectomy”; "open gastrectomy for advanced gastric cancer”, resulting
in 4183 studies found (Figure 1).
Inclusion criteria determined that only systematic reviews and clinical
trials, published between 2011 and 2016 and reporting adenocarcinoma as
histological finding for gastric cancer were used.
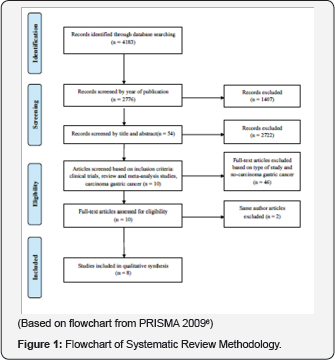
Exclusion criteria eliminated cohort, observational
studies, case-control and case reports, published more than five years
from date of research and that reported other histological types of
gastric cancer besides adenocarcinoma. For articles published by the
same author, only the most recent were considered. The research, after
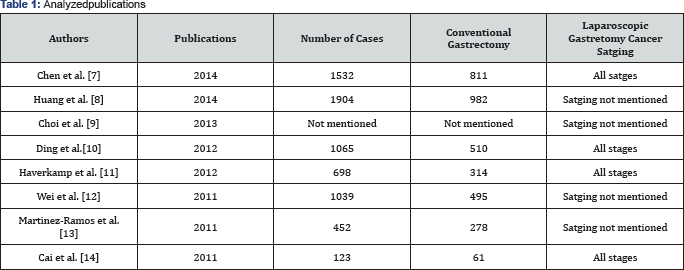
the application of the above-mentioned parameters resulted in eight
articles (Table 1).
Results
A study performed by Chen et al. [7]
compared the laparoscopic and laparotomic approaches. It evaluated
articles published until 2014, finding 14 suitable publications (1
randomized clinical trial and 13 observational studies). It covered 1532
patients from nine different regions (Italy, Belgium, France, USA,
Chile, South Korea, Japan, Taiwan and Hong Kong), being 721 submitted to
laparoscopy and 811 to laparotomy. By the end of the study, the
conclusion was that the bleeding and need for transfusion, necessity of
painkillers, recovery of gastrointestinal functions, dietary restart and
the number of complications (cardiorespiratory, metabolic, pulmonary
embolism/deep venous embolism and non-surgical infections) were smaller
regarding the patients submitted to the laparoscopic approach. Also, the
duration of hospitalizations proved to be, in average, 3,75 days
smaller for those patients. Nevertheless, the conventional - laparotomic
- approach presents shorter surgical time. Parameters such as: number
of resected lymph nodes, distal and proximal margins, taxes of surgical
related complications (regarding anastomosis, intrabdominal collections,
bleeding, surgical wound and delayed gastric emptying, among others),
mortality and morbidity taxes did not present a different result
comparing both approaches. The recurrence of tumors was seen in 22,7% of
the laparoscopic gastrectomies and in 21,9% of the laparotomic, not
representing a considerable statistical difference according to the
results of the study.
Huan et al. [8]
selected 11 articles for their systematic revision, published between
January 2000 and September 2013. A total of 1904 gastrectomies with D2
lymphadenectomy were analyzed, 982 of them being performed via
laparoscopy and 922 via laparotomy. A statistical equivalence was seen
regarding survival rates, bleeding and complications. Surgical time was
shorter for the conventional approach and infectious complications were
seen in smaller proportion on patients submitted to laparoscopy.
The systematic review published by Yoon Young Choi et al. [9]
analyzed 10 other studies (9 cohort and one randomized clinical trial).
The authors concluded that there was no statistical difference when
comparing average survival rate or free of disease survival rate for
both laparoscopic and laparotomic approaches.
Ding et al. [10]
analyzed eight retrospective case- control studies, with a total of
1065 gastrectomies with D2 lymphadenectomy, 510 laparoscopic and 555
conventional ones. Regarding the decrease of use of painkillers, they
concluded that the minimally invasive procedure had an advantage
compared to the conventional surgery. However, the studies were not
capable to show whether the lymphadenectomy performed during the
laparosocopic gastrectomy is adequate or its long term prognostic.
Another disadvantage seen, was the increase in the surgical time and the
requirement of more experienced surgeons and more developed technology.
As advantages, the laparoscopy showed less complication rates and fewer
hospitalization days.
Haverkamp's [11]
review included eight randomized clinical trials. Compared to the
conventional approach, the laparoscopy is associated with a considerable
reduction of post-surgical complications, bleeding and time of
hospitalization. In other hand, the study reinforces the need of better
studies to evaluate the mortality rates, resection margins and number of
resected lymph nodes.
The meta-analysis written by Wei [12]
evaluated ten studies published between the years of 2001 to 2010,
being classified as one clinical trial and nine case-controls. It
comprised 1039 patients, 495 submitted to gastrectomy via laparoscopy
and 544 via laparotomy The number of resected lymph nodes, the
anastomotic leak and the survival rates in 5 years had no major
differences between the two methods. They concluded yet that the
bleeding, need of painkillers, reestablishment of gastrointestinal
function, length of hospitalization and surgical wound infection were
lower in patients submitted to LG. Still, the average surgical time of
the conventional approach was around 57,14 minutes shorter.
The Spanish meta-analysis of Martinez-Ramos [13]
analyzed seven clinical trials (one of them randomized). The total of
assessed patients were 452, with 174 laparoscopic gastrectomies
performed. The bleeding volume during the laparoscopic approach was
122mL smaller in average and the hospitalization took around 6 days less
when compared to open gastrectomy. Nevertheless, the CG took 44min less
to be performed, in general. The number of resected lymph nodes was
statistically similar in both approaches. In the same way, the survival
rate in 5 years showed not to differ in both groups.
In 2011, Cai et al. [14]
published a randomized clinical trial comparing LG and CG in patients
diagnosed with advanced staged gastric cancer. Between March 2009 and
December 2010, 123 patients were evaluated. Sixty two of them were
submitted to LG and 62 to CG. According to the authors, the first
approach shower smaller morbidity and mortality rates, less
complications and lesser hospitalization time. However, CG still had a
faster length of performance. The study showed no statistical
differences regarding survival rates.
Discussion
According to the publications analyzed, the only
parameter in which CG was superior to LG was regarding surgical length.
Many authors justify this difference by saying that the minimally
invasive procedure has a higher complexity of performance of the
gastrointestinal transit reconstruction, as well as the more complex
lymphadenectomy. It is also take into account the preparing of materials
and laparoscopic instruments, the decrease of tactical sensation and
the different levels of expertise of the surgeons performing the
procedure [7-14].
The incidence of bleeding and need of transfusion
were smaller when the laparoscopic approach was utilized. That occurs
due to better visualization of vascularization and better instruments
available [7,11,13]. Only one of the mentioned articles concluded that the bleeding incidence in both procedures was similar [9].
There was a decrease on the need of use of
painkillers and lower complication rates in the groups submitted to
gastrectomy via laparoscopy, that fact is justified by the minimally
invasive type of approach [7-11,14].
The early reestablishment of gastrointestinal function, evaluated by the elimination of flatulence by the patients [7,12],
associated with an early progression of diet7 occurs due to less
mobilization of the intrabdominal cavity, with formation of looser
adhesions, leading to a reduced ileus.
The results of reduced hospitalization time seen in patients submitted to laparoscopic gastrectomy [7,11-14],
it may occur due to minimal manipulation of the intestines leading to
early reestablishment of gastrointestinal function, reductions of
inflammatory reaction and fast return to daily activities.
Regarding the number of resected lymph nodes and of
tumoral recurrence and survival rates, both techniques showed no
statistical differences [7-9,12-14].
This conclusion is only possible due to comparisons between experienced
surgeons, being this level of expertise acquired approximately after 40
performed surgeries6. One of the studies concludes that further
investigation is necessary to define which approach is most advantageous
on the matter of lymph node resection. Two articles also mention the
need for more studies to obtain a certain level of oncological safety
for the extrapolation of the recurrence and survival rates obtained [7,13].
Two of the parameters analyzed showed no consensus
between two revisions: tumor resection margin and morbidity and
mortality rates. As for the resection margins, a study [7]
did not find a statistically significant difference in this regard when
compared the two gastrectomy techniques. Another article says more
studies may be needed to better define the resection margin standards [11].
As for the morbidity and mortality rates, no definite
conclusion could be made. One of the revisions showed no statistical
difference in the criteria for the two surgical approaches [7]; another claims the laparoscopic technique to be the one with lower morbidity and mortality [14];
and still, another review infers the need for further studies to be
performed to determine the rates for each type of approach [15].
In addition to the revisions mentioned above, there are yet two ongoing randomized clinical trials. The KLASS-02 study [15]
covers 1050 patients equally divided (525) between the groups submitted
to laparoscopic and conventional gastrectomy. Participants with early
staged gastric cancer, with muscularispropria invasion, but not adjacent
organs invaded (T2 to T4), with no lymph node or limited to perigastric
lymph nodes metastasis were selected for this study. The authors aim to
demonstrate that there is no inferiority of the laparoscopic approach
in the free of disease rate in 3 years.
The second ongoing study is the LOGIC-trial [16].
In this trial, 210 participants with surgically resectable gastric
cancer (T1-4b, N0-3b, M0) are divided equally between the two groups
(laparoscopy X conventional gastrectomy). It aims to demonstrate that
laparoscopic gastrectomy has the same benefits to patients provided by
the conventional technique, but with less blood loss during the surgery,
lower complication rates and shorter hospitalization period.
Finally, a systematic review with meta-analysis performed by Zhang [4]
compared two techniques in laparoscopic gastric cancer approach:
assisted laparoscopic gastrectomy and the totally laparoscopic
technique. The study included 12 observational studies with 2255
patients (1228 submitted to ALG and 1027 submitted to the TLG). They
concluded that bleeding and hospitalization period were lower in the
fully laparoscopic technique. The rest of the parameters analyzed, such
as: time of surgery, the number of lymph nodes resected, the need for
painkillers, time for elimination of flatulence, dietary reintroduction,
morbidity and complication rates with anastomoses showed no significant
differences between the two techniques. In this study, the authors did
not mention the cancer staging of the patients operated.
Conclusion and Final Considerations
Based on all the analyzed reviews, the laparoscopic
gastrectomy proved to be as viable as the conventional technique when
opted for approach of a gastric adenocarcinoma, presenting, in the
majority of parameters, better results than those of open surgery. It
must be expected that even the laparoscopic technique is bound to
further development in the future, being performed by single incision
even [17,18]. Nevertheless, some considerations are still necessary.
Most studies do not have a clear definition of
locally advanced cancer, having the majority of them not mentioned the
stages of gastric cancer of the patients operated, causing a great
impairment for definitive conclusion about the viability of the
laparoscopic technique for the disease, despite the positive results.
Furthermore, due to the fact that each systematic review assessed a
limited number of studies (with an exception of the randomized clinical
trials), they present lower levels of evidence and the results might not
truly match with the reality. Factors such as the lack randomization of
participants, unexperienced surgeons, small samples, large
heterogeneity between groups and short postoperative follow-up have to
be taken into consideration.
Therefore, it is recommended to wait for the
conclusions of the ongoing clinical trials. Moreover, even stimulate new
studies using AJCC's gastric cancer staging, in order to achieve
greater impact for the medical and scientific community.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment