When Should Thiopurine Therapy During Sustained Remission in Inflammatory Bowel Disease be Stopped?_Juniper Publishers
Authored by Marisa Iborra
Abstract
Azathioprine is effective for maintenance of
remission in inflammatory bowel disease, nonetheless, duration of
efficacy and the dose response relationship has not been fully
evaluated. Currently, there are no general recommendations yet that can
help us selecting patients who would benefit from the discontinuation of
TP without an increased relapse risk.
Abbreviations: AZA: Azathioprine; IBD:Inflammatory Bowel Disease; CD: Crohn's Disease; UC: Ulcerative Colitis; anti-TNF: Anti-Tumour Necrosis Factor
Introduction
Azathioprine (AZA) have been used in clinical
practice for more than 50 years and remain the mainstay of maintenance
treatment for inflammatory bowel disease (IBD), either as alone and/or
in combination with anti-tumour necrosis factor (anti-TNF) drugs [1]. Today, Thiopurine have demonstrated their capacity maintaining remission in the long-term in both Crohn's disease (CD) [2,3] and ulcerative colitis (UC) [4,5], and it seems that the effect does not disappear after for up to 5 years [6]. Moreover, during follow-up responders had a significantly reduced risk of intestinal surgery and perianal surgery [7].
Discussion
Despite increasing evidence of safety from several
studies, a percentage of responders developed cancers, including
nonmelanoma skin cancers [7,8].
A rare and usually fatal lymphoma, hepatosplenic T-cell lymphoma, has
been related with younger IBD patients who received long-term therapy
(at least 2 years) with Thiopurine [9]. Thiopurine use in IBD appears to be strongly related with an increased risk of Epstein-BARGH virus-positive lymphoma [10,11].
Recently, it has been linked immunosuppressive treatment with
opportunistic infections during severe lymphopenia in IBD patients [12].
Regular monitoring of blood counts and liver test is required in order
to early detection of bone mARGHow and liver toxicities [13,14].
Treatment strategies have changed accordingly.
Presently, the early introduction of Immuno modulators and anti- TNF
therapy targeting a window of opportunity before the development of
potentially intestinal complications and they are capable of change the
disease evolution. However, the clinicians unknown the best moment of
therapy stopping once remission is achieved. Identifying IBD patients
with increased risk of relapse after Thiopurine withdrawal during
sustained clinical remission is essential for appropriate management.
From a clinical point of view, our patients are young
and have a long life expectancy. Physicians should consider maintaining
thiopurinesonly in cases in which a clear benefit is expected. On the
other hand, whether or not AZA can be stopped is an important question
and factors involved in the decision to removal the drug in patients
with IBD are necessary. Previous retrospective study suggested that the
risk of relapse appeared to be similar if we withdrawal or maintain AZA
after 4 years of remission in CD patients [15]. In Table 1
you can see the most relevant studies assessing relapse rate in IBD
patients under immuno suppressive therapy in case of discontinuation as
well as the predictive factors.
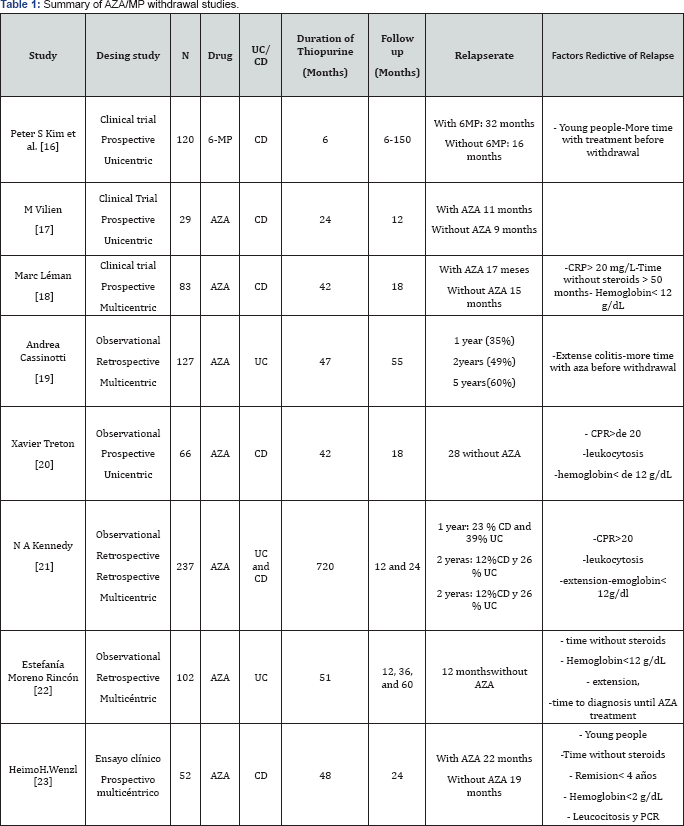
AZA (Azathioprine), 6-MP (6 mercaptopurine), CPR ( C reactive protein), UC (ulcerative colitis), CD (Crohn's disease)
Conclusion
In conclusion, Thiopurine withdrawal in the context
of sustained remission is associated with a high risk of relapse.
Currently discontinuation of AZA may be considered after 4 years in IBD
patients in sustained remission and steroid free [24,25].
Further investigations are necessary in order to identify risk factors
of relapse after stopping immunosuppressive therapy The safety and
actual risk/benefit ratio of therapy withdrawal needs to be studied in
prospective controlled trials, given the need to optimize the use and
duration of potentially risky and costly therapies.
Conflict of Interest
No financial support was received for the preparation of this study. The authors declare that no conflict of interest exists.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment