The Profile of Food Protein Allergy in Children below 2 Years in Eastern India–An Observational Study_Juniper Publishers
Authored by Bhaswati C Acharyya
Food allergy has been referred to as the second wave of the allergy epidemic, asthma being the first [1].
Incidence of food protein allergy, especially cow’s milk protein
allergy Is on a rise In India. The aim of this study was to find out the
presentation, cross allergy and outcome after treatment of the infants
and children below 2 years of age who had been diagnosed with food
protein allergy, in a tertiary centre of Eastern India.
Materials and Methods
A retrospective study was undertaken where the case
files of children below 2 years, who were diagnosed to have food protein
allergy between the years March 2014 to Dec 2015, were analysed. These
children were reviewed in the Paediatric Gastroenterology department of a
tertiary centre in Kolkata. Upper GI Endoscopy,
Sigmoidoscopy/colonoscopy and immunoglobulin E against Cow’s milk
protein (using Immunocap Allergy test modality) were used as diagnostic
modalities. Celiac screening was done in all patients above 6 months who
were already exposed to wheat. Endoscopic diagnosis of food protein
allergy was based on characteristic intestinal biopsy (>6
eosinophils/HPF in recto sigmoid and >20 eosinophils/HPF in duodenal
and Gastric biopsies and >15 eosinophil /HPF in oesophageal
biopsies).
Results
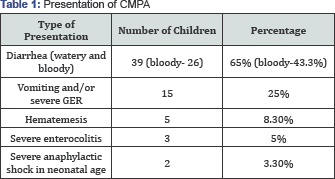
60 children (26 males and 36 below 1year of age) have
been diagnosed with food protein allergy among a total of 120
children(less than 2 years) attending clinic with GI symptoms. Mean age
was 9+2 months and median duration of symptoms ware 5.5 months. Vomiting
and or severe gastro esophageal reflux disease was presentation in 15
(25% patients). Haematemesis was presentation in 5 (8.3%) infants.
DiARGHhoea (watery and Bloody ) was present in 39(65%) children and
amongst them 26(43.3%) had bloody diARGHhoea . 2(3.3%) infants presented
with severe anaphylactic shock in neonatal age group and severe
enterocolitis was presenting feature in 3 infants (5%). Duodenal
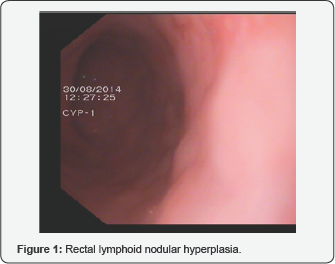
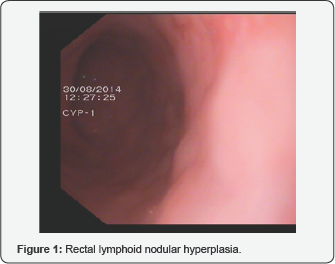
lymphoid nodular hyperplasia was the finding in 80% cases presenting
with vomiting. Ulcerative procto-colitis with or without lymphoid
nodular hyperplasia was the finding in all cases (100%) of bloody
diARGHhea (Figure 1& 2).
IgE against cow’s milk protein (Immunocap) was positive in 3 patients
(5%) (Evaluated in 12 patients). Cow’s milk was excluded from the diet
for all children. Hydrolysed infant formula was used in infants below 6
months. Peptide based formula and soya formula were used in rest. 10
(16.6%) patients were found to be cross allergic to Soya protein. 2 were
found allergic to Chicken protein. Celiac screen was positive in a boy
of 20 months who also had eosinophilic proctocolitis and was kept on
Peptide based formula and gluten free diet. Median duration of milk
exclusion was 18 months. All patients were followed up monthly for 2
months, 2 monthly for three visits and 3 monthly thereafter until 18
months in total since diagnosis. Milk challenge was not done routinely.
Accidental milk in mother's diet caused recurrence of symptoms in 5
patients when done within 1 year While 8 patients are still on milk
exclusion rest 50 patients did well after gradual introduction of milk
after 18 months of restriction. 2 were lost in follow up (Table 1, Figure 1& 2).
Discussion
Food allergies affect 68% of infants younger than 2
years. In a cohort of 1,749 newborns from the municipality of Odense in
Denmark who were prospectively monitored for the development of cow’s
milk protein intolerance during the first year of life, a 1 year
incidence of 2.2% was reported [2].
Varying incidences of specific intolerances have been reported in
different countries. Whether these differences are due to genetic or
cultural factors is unclear [3].Cow’s
milk, the commonest food has been shown to be the common cause of
chronic diARGHhea in children <3 years of age in India [4].
DiARGHhoea was the commonest presentation of CMPA in
our study (65% with 43.3% bloody diARGHhoea) which is similar to the
study of Poddar et al who also showed diARGHhea as commonest
presentation (90%) and 2/3rd was large bowel diARGHhea [4]. Rectal bleeding is a common manifestation of CMPA [5].
Therefore, CMPA should always be the first possibility in infants with
rectal bleeding, over and above rectal polyp, as the latter is less
common in infancy [6].
Sigmoidoscopy was diagnostic in 100% cases of bloody
diARGHhea and about 82% cases of diARGHhea in our study which was
similar to the other study [7].
It has been shown that on cow’s milk withdrawal there is rapid reversal
of histopathological changes and on re-exposure to milk there is rapid
deterioration in 24-48 hours [8].
In previous studies re-challenge with milk was done after 3 months in 80% of cases showing positive results [7].
But in our study routine re-challenge was not done but accidental milk
in mother's diet caused recurrence of symptoms in 5 patients when done
within 1 year. A total of 18 months restriction has been advocated for
all patients.
Conclusion
Food protein allergy especially CMPA is now a common
entity in India. This study also confirms that Cow’s Milk Protein
Allergy is an existing entity in the young population below 2 years in
the eastern part of India as well. High index of suspicion and
appropriate referral can achieve early diagnosis and symptomatic relief.
Gradual introduction of food protein after adequate period of
restriction is successful in most of the cases.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment