Perspectives on Mechanical Small Bowel Obstruction in Adults_Juniper Publishers
Authored by Elroy Patrick Weledji
Abstract
Small bowel obstruction is a serious and costly
medical condition indicating often emergency surgery. Delay in operative
intervention may lead to an unnecessary bowel resection, an increased
risk of perforation and an overall worsening of patient morbidity and
mortality. A thorough history and examination would distinguish simple
from strangulation obstruction and facilitate appropriate management.
The article reviewed small bowel obstruction and emphasized the
importance of history taking and examination in the early diagnosis of
its cause, thus, facilitating appropriate management.
Keywords: Small bowel; Obstruction; Mechanical; Clinical features; TreatmentIntroduction
Small bowel obstruction accounts for about 85% of
cases of intestinal colic and the other 15% are due to large bowel
obstruction [1].
It is a serious and costly medical condition constituting 1.9% of all
hospital and 3.5% of all emergency treatment that has led to laparotomy
in the United States [2-4].
The main clinical issue is to determine whether the obstruction affects
the small bowel or the colon, since the causes and treatments are
different. Delay in operative intervention may lead to an unnecessary
bowel resection, an increased risk of perforation and an overall
worsening of patient morbidity and mortality. The overall mortality is
approximately 10% and is greatest in patients with ischaemic bowel which
may or may not have perforated prior to surgery [2,5,6]. The most common causes of death are intra-abdominal sepsis, myocardial infarction and pulmonary embolism [1-6].
Intestinal obstruction may be mechanical which presents with colicky
pain or paralytic which is painless being aperistaltic. The latter is
commonly seen in postoperative ileus which resolves after 24-48 hrs or
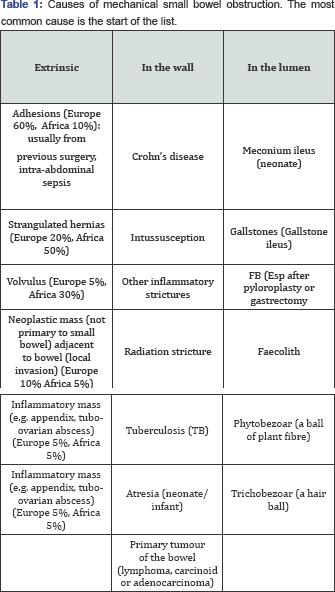
from electrolyte (potassium) imbalance with diuretic use [6,7]. Mechanical obstruction may be due to obstruction in the wall, in the lumen or outside the wall of the bowel (Table 1) [2].
There is a degree of overlap as mechanical obstruction can progress to
paralytic obstruction (ileus) as it becomes more severe. Small bowel
obstruction may be simple obstruction that can wait for 24hrs or
strangulating obstruction (closed-loop) where there is interruption of
the blood supply of the bowel requiring an immediate operation [2,6-10].
Discussion
The visceral pain of intestinal colic is from
increased peristalsis against the obstructive lesion is usually referred
towards the midline rather than being localised as the gut has a
midline origin of development. The visceral sensory fibres are cARGHied
by the sympathetic nerves on their way to the spinal cord. The
consequences of bowel obstruction are progressive dehydration,
electrolyte imbalance and systemic toxicity due to migration of toxins
and bacteria translocation either through the intact but ischaemic bowel
or through a perforation [2,5].
Aetiology of Small bowel obstruction
There are several possible causes and the
epidemiology varies considerably from region to region. Adhesions is the
cause in 80% of instances. They are usually from previous abdominal
surgery and the use of abdominal mopping gauze swabs or towels [11-15], but may also arise from previous intraabdominal sepsis [11,12,14].
They produce kinking of the bowel or obstruction from pressure of a
band or volvulus. Intestinal adhesions are the commonest cause of
mechanical small bowel obstruction in the western world due to the
greater number of operations performed [2,11].
Intestinal adhesions to other vascular structures occur as injured
peritoneal cavity need to gain some extra blood supply during the
healing process [12-14].
Thus by minimizing disruption of the peritoneal cavity
minimially-invasive surgery can help reduce the probability of adhesion
formation [15].
Inguinal hernias are the commonest cause of mechanical small bowel
obstruction in the developing world where the uptake of modern medicine
is low with the consequent delay in surgical interventions [16].
Usually pressure of the neck of the sac causes obstruction especially
with the nARGHow femoral and indirect inguinal hernia defects and
occasionally internal hernia, and, it may be associated with
strangulation. Primary small bowel volvulus is a life-threatening
surgical emergency requiring immediate laparotomy following
resuscitation. It occurs in the 'virgin' abdomen with no anatomic
abnormalities nor predisposing factors. It is often seen in Africa and
Asia, and seems to be associated with special dietary habits (high fibre
diet) especially after a fast causing the incipient weight of the
terminal ileum to rotate round the short base of the mesentery. The main
problem is to differentiate it from other causes of obstruction that
can be treated conservatively Central abdominal pain resistant to
narcotic analgesia should heighten the suspicion of the diagnosis [17].
Rarer causes of small bowel obstruction are neoplasms (usually
metastastic and thus extrinsic) as primary small bowel malignancy is
rare. Intussusception in adults is rare and always require a laparotomy
as it is commonly due to an underlying malignancy such as lymphoma or
carcinoma. Any inflammatory mass such as diverticular, appendiceal,
tubo-ovarian ileo-caecalCrohn'setc, may cause small bowel obstruction by
blocking the ileocaecal valve or by causing a localized ileus [18,19].
The nARGHowest part of the small bowel is the terminal ileum which is
the preferred site of obstruction by most of the luminal causes. A right
iliac fossa mass in a patient with iron- deficiency anaemia from an
occult chronic bleeding is caecal carcinoma or other malignancy until
proven otherwise. These patients require computer tomography (CT)
scanning±colonoscopy for further elucidation [2,19].
Luminal obstruction from gallstone (gallstone ileus), hair
(trichobezoar), vegetable matter (phytobezoar) or foreign objects are
rare [19].
The rare patient with a Richter's hernia in which only the
antimesenteric portion of the small bowel is trapped without bowel
obstruction may be undetected on physical examination, and, patients
with partial obstruction can be considered at minimal risk of
strangulation. Rarely small bowel obstruction can be caused by internal
hernias related to mesenteric defects or recesses [9].
A modern clinical example is the internal hernias that develop after a
laparoscopic gastric bypass in which small mesenteric defects
(transversemesocolon, enteroenterotomy or behind the Roux limb can be
created and there are fewer adhesions to tether small bowel loops and
prevent them from herniating causing obstruction and potentially
strangulation. In addition patients who have greater degrees of weight
loss after laparoscopic Roux-en-Y gastric bypass may be more prone to
internal hernia because of loss of the protective space-occupying effect
of mesenteric fat [10].
How to tell the aetiology, level and severity of obstruction preoperatively?
The four cardinal clinical features of intestinal
obstruction are colicky abdominal pain, vomiting, constipation and
abdominal distension. The history, examination and investigation will
help tell the aetiology, level and severity of the obstruction. These
have considerable bearing on the indications for operation, and on the
necessary preoperative preparation.
History: The onset of the obstructive symptoms
is usually sudden with high small bowel obstruction but more gradual
with low small bowel obstruction. The colicky pain comes with greater
frequency in high small bowel obstruction, about every 5 minutes in
jejunal obstruction, but every 30minutes in ileal and colonic
obstruction. The pain is typically central in small bowel obstruction
but where strangulation of the bowel has occurred the pain may become
constant and localised. If the colic is in the lower abdomen it is more
likely to be due to colon obstruction. Vomiting follows the pain and for
high obstructions vomiting is more profuse and occurs earlier.
Initially food contents are vomited but later the vomit becomes
faeculent (brown and foul smelling) [1,2,19]. The 24 hour secretory function of the proximal gut is illustrated in Table 2. It gives an indication of the amount of fluid that can be sequestered in the intestines or lost in the vomitus [2,6].
The clinical history may establish other features indicative of the
likely aetiology of the obstruction. A history of abdominal surgery may
suggest adhesive small bowel obstruction. A past history of colorectal
or other intra-abdominal malignancy, recent alteration in bowel habit or
the passage of blood is suggestive of neoplasm.

Examination: The examination findings will
depend on the stage at which the patient presents. The patient with
complete obstruction (no passage of flatus and faeces) are at
substantial risk of strangulation (20-40%) but a patient with chronic
obstruction may appear generally quite well with normal vital signs [20].
On the other hand the patient who has an acute closed- loop small bowel
obstruction may be profoundly ill, toxic, tachycardic, pyrexic and may
have a leucocytosis at the time of presentation [21].
A tense, tender, irreducible lump with no cough impulse especially over
a hernia orifice with often erythema of the skin is strangulation until
proven otherwise. Occasionally, the hernia is internal and not palpable
[20,21].
The physical findings would include dehydration, abdominal distension
and sometimes visible peristalsis. Dehydration assessed by examination
of the mucous membranes and skin turgor is an indication of severe fluid
depletion which is more marked in high than low small bowel
obstruction. Abdominal distension is usually evident and more marked the
more distal the obstruction, but it is more an indication of the site
than the extent of obstruction. Swallowed air, gas from bacterial
fermentation and nitrogen diffusion from the congested mucosa are all
responsible for the increased intestinal gas [5,6].
The abdominal distension is minimal in high small bowel obstruction and
more prominent in low. In low small bowel obstruction distension is
mainly central. In colonic obstruction distension is mainly in the
flanks and upper abdomen. Abdominal distension may be so marked as to
render further assessment of the intraabdominal contents impossible. The
cause of the obstruction may be evident (e.g. scars from previous
surgery, a tender irreducible hernia, an abdominal mass e.g.
intussuception or carcinoma of bowel) [5,6,12].
Rarely a mass be felt, or an irregular enlarged liver may suggest a
malignant lesion as the cause of obstruction.Percussion produces a
tympanic note and auscultation high- pitched tinkling, long-lasting
bowel sounds. If the obstruction is advanced there may be signs of bowel
strangulation (worsening constant pain, toxic patient, tachycardia,
hypotension and pyrexia) with reduced or absent bowel sounds (paralytic
ileus) [1,6].
It may be clinically difficult to distinguish with any certainty
between simple obstruction and strangulation but the later condition is
obviously very serious if overlooked [6,20].
Simple obstruction presents with colicky (visceral) pain but no pain
(somatic) on coughing as sign of peritonism. However, there is mild
generalized abdominal tenderness from the distension with gas and fluid.
Strangulation (closed-loop) obstruction usually has an acute onset of
severe pain which is constant and associated with cough peritonism [21].
Digital rectal examination is mandatory in intestinal obstruction
although rectal cancer is a rare cause of intestinal (large bowel)
obstruction unless very advanced. Assessment of the cardiovascular and
respiratory systems is necessary in small bowel obstruction as most of
these patients will require surgery [6].
Treatment of small bowel obstruction
In the past 15 years, there have only been some modest progress and advancement in the treatment of small bowel obstruction [2,4,6].
It has been demonstrated convincingly by the NCEPOD (National
Confidential Enquiry into Perioperative Deaths) that patients with
intestinal obstruction who are hypovolaemic have a higher morbidity and
mortality if not adequately resuscitated prior to surgery [22].
This is exacerbated by the vasodilation of anaesthesia which may cause
catastrophic hypotension and renal failure. Treatment commences with
resuscitation by correcting fluid and electrolyte deficits, nasogastric
tube decompression and analgesia. There is careful monitoring with fluid
balance charts, pulse and blood pressure as resuscitation is continued
until the central venous pressure is restored and a consistent adequate
urinary output of atleast 30mls/hr for an average 70kg patient [2,6,23]. The management of simple obstruction may be either operation or observation depending on the likely cause [24].
If simple obstruction is thought to be due to adhesions conservative
treatment is initially indicated as spontaneous resolution will occur in
up to 70% of patients with obstruction secondary to adhesion [2,6].
Surgical intervention is necessary when conservative treatment with
nasogastric decompression and intravenous fluid resuscitation fails
after 48hrs as the patient should not remain obstructed for more than
that length of time, or with evidence of peritonitis from strangulation
obstruction [2,24,25]. Conservative treatment often succeeds in postoperative obstruction from adhesions or ileus [25]. Conservative treatment may be appropriate for inoperable carcinomatosisperitonei.
Operation is indicated for
a) Strangulation obstruction as soon as patient is
rendered fit. The overall operative mortality for strangulated hernia is
10% and so adequate preoperative resuscitation is crucial [2,22-24,26];
b) Obstruction due to some cause that will not
settle e.g. obstructed hernia, carcinoma, gallstone ileus etc. In the
latter, the obstructing gallstone is removed either by expression or by
the use of stone-holding forceps via a proximal transverse enterotomy
which is repaired by two layers of suture. The chronic
cholecystoduodenal fistula is left undisturbed [2,6].
c) Simple obstruction that fails to settle on
conservative treatment. The presence of fever and leucocytosis should
prompt inclusion of antibiotics in the initial treatment regimen. After
relieving the cause of the obstruction by operative intervention, it is
usually necessary to decompress the stomach and the greater part of the
small bowel by nasogastric drainage. Intestinal peristalsis is inhibited
by gastric distension, and is restored when this is relieved.
Antibiotic prophylaxis is usually necessary if obstructed intestine has
been opened [2,6,26,27].
Conclusion
Small bowel obstruction remains a common and
difficult problem encountered by the abdominal surgeon. Following
resuscitation a precise history may indicate the pathology and physical
examination supported by basic imaging may indicate where the pathology
is. These have considerable bearing on the indications, timing of
intervention, and necessary preparation should operation be considered.
Appreciation of fluid balance, acid-base-electrolyte disturbance and the
importance of preoperative resuscitation decrease the morbidity and
mortality from intestinal obstruction. Advances in minimally- invasive
surgery would help minimize adhesion formation, the commonest cause of
intestinal obstruction.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment