Unusual Cause of Dysphagia in a Middle Age Male
Authored by Zaheer Nabi
Abstract
Dysphagia is not uncommon in gastroenterology
practice. The differential diagnosis is wide and includes both
mechanical and motility causes. Esophageal lichen planus is uncommon but
now increasingly recognized. It occurs in more than half of cases of
lichen planus with muco-cutaneous involvement. Often there is a delay in
diagnosis and subsequent treatment. The endoscopic picture of
esophageal lichen planus closely mimics that of eosinophilic
esophagitis. However, histological picture is entirely different and
useful for differentiating between the two. We present here a
challenging case where characteristic oral lesions provided with the
first clue to the diagnosis of esophageal lichen planus. Subsequent
histo-pathological findings were characteristic and confirmed the
diagnosis.
Keywords: Dysphagia; Endoscopy; Lichen planus Introduction
Lichen planus is a well-recognized chronic idiopathic
disorder involving the skin, nails and mucosal surfaces including the
mouth, pharynx and perineum. Mucosal surface involvement is found in
about 30%-70% of patients diagnosed with lichen planus [1]. Oesophageal
involvement is rare and its true prevalence is unknown. In this case
report we describe a middle aged gentleman presenting with symptoms of
gastroesophageal reflux disease and diagnosed as oesophageal lichen
planus on complete evaluation.
Case Report
A 44-year-old man presented with heartburn,
occasional pain and difficulty in swallowing solid foods for 3 years.
There was increase in severity of symptoms for last 1 year during which
he lost about 8kgs weight. There was no relief of symptoms with antacids
or proton pump inhibitors. There was no past history of asthma, atopy
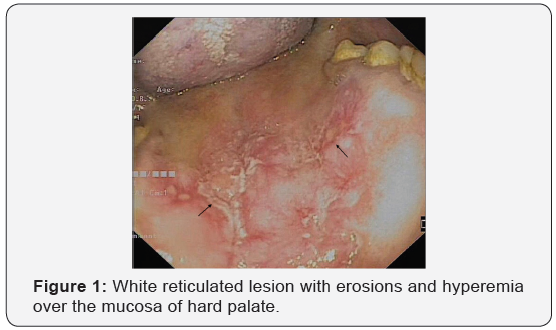
or allergy. Oral examination revealed white reticulated lesion with
erosions and hyperemia over the mucosa of hard palate (Figure 1). There
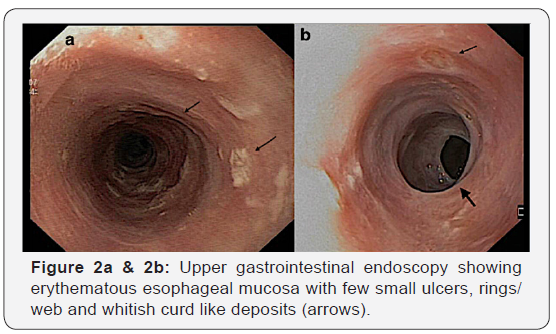
were no skin lesions. Upper gastrointestinal endoscopy showed
erythematous esophageal
mucosa with few small ulcers, rings/web and whitish curd like deposits
(Figure 2a & 2b) involving predominantly upper
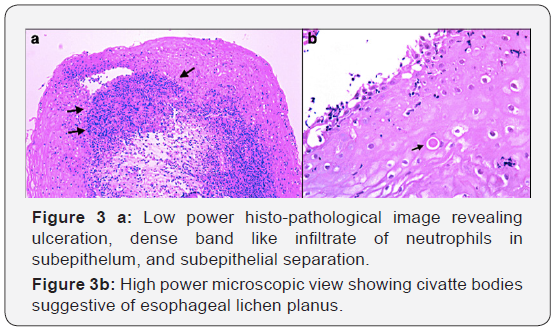
and mid esophagus. Histopathology of the esophageal lesions revealed
ulceration, dense band like infiltrate of neutrophils in subepithelum,
civatte bodies and subepithelial separation suggestive of esophageal
lichen planus (Figure 3a & 3b). He was initially treated
withswallowed fluticasone for 4 weeks, but there was no symptomatic
relief. Subsequently he was started on oral steroids in tapering
fashion.There was significant clinical improvement and follow up
endoscopy at 4 weeks revealed healing of esophageal lesions.
Discussion
Esophageal lichen planus is considered to be rare. However,
the true prevalence of lichen planus esophagitis among patients
with oral lichen planus may have been underestimated because
of subtle clinical findings and lack of characteristic histological
features. In a recent study, chromoendoscopy was used to
determine the prevalence of esophageal involvement in patients
with oro-cutaneous lichen planus. Up to 50% of patients with
oro-cutaneous lichen planus had esophageal involvement [2]. In
another study, esophageal involvement was found in about 60%
caseswith LP of the skin, hair, nails, oral mucosa, and/or genital
mucosa [3]. Early recognizing of esophageal involvement is
necessary to prevent development of strictures [4]. Also several
case reports have described the development of squamous
cell carcinoma in these patients [5,6]. However, the optimal
surveillance interval is not known in these patients.
Most of the described cases in literature are middle aged
females. Clinically patients may be asymptomatic or present
with dysphagia and odynophagia. Endoscopically there may be inflamed friable mucosa, webs, pseudomembranes, erosions,
ulcerations or even strictures in late cases. Clinical and
endoscopic picture of esophageal lichen planus may mimic that
of eosinophilic esophagitis. Histological features in esophageal
lichen planus include band like or lichenoid lymphocytic infiltrate
involving the superficial lamina propria and basal epithelium,
basal keratinocyte degeneration which often include Civatte
bodies (necrotic keratinocytes with anucleate remnants) [7].
Unfortunately, there is no standard treatment for oesophageal
lichen planus. However, early treatment may prevent formation
of strictures.
Treatment options based on previous reports
include swallowed fluticasone, oral steroids or other
immunosuppressants like tacrolimus and cyclosporine [8]. In a
recent report, topical swallowed budesonide or fluticasone was
effective for oesophageal lichen planus [9].
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment