Association between Nonalcoholic Fatty Liver Disease and Carotid Atherosclerosis-Juniper Publishers
Abstract
Aim/Background: Nonalcoholic
fatty liver disease (NAFLD) frequently accompanies to the criteria of
Metabolic Syndrome (MetS) like obesity, diabetes, and dyslipidemia. It
is recently approved as a liver attaint of MetS. While MetS is a highly
atherogenic condition we examined whether NAFLD was associated with
atherosclerosis, as measured by ultrasound in the carotid arteries.
Methods: Carotid
intima-media thickness and cardiovascular risk factors were evaluated in
64 patients with an ultrasound diagnosis of primary NAFLD and 64
matched population controls. Metabolic syndrome was established
according to WHO and ATP-III criteria. IMT values were evaluated
according to protocols of standard measurements of carotid artery.
Results: The metabolic syndrome
and all its individual features were significantly (P<0.001) more
frequent in NAFLD patients than in control subjects. Patients with NAFLD
and controls had similar mean intima-media thickness (IMT) of 1,06±0,71
mm and 0,96±0,66 mm respectively, but plaque prevalence was
significantly higher in patients with NAFLD than in controls (18,7% and
9,37%, respectively). Conversely, C-reactive protein levels were
elevated in control group comparing to patient group.
Conclusion: In the present study
NAFLD did not have increased IMT but had high prevalance of carotid
plaque. The presence of MetS did not affect the prevalance of increased
IMT and carotid plaque formation. The clinical implication of this study
is that patients with NAFLD and control group are at similar risk of
CVD. Studies in large NAFLD patient population comparing to control
goups should be performed. How be it, patients with NAFLD should undergo
periodic cardiovascular risk assessment.
Keywords: NAFLD; Carotid atherosclerosisIntroduction
Nonalcoholic fatty liver disease is described with
fat accumulation in the liver without significant amount of alcohol
consumption and has a spectrum ranging from simple steatosis to
steatohepatitis, cirrhosis and liver failure [1-2]. NAFLD frequently has
a relation to the components of metabolic syndrome like diabetes,
dyslipidemia, obesity and hypertension [3-4].
Because of associated metabolic disturbances, NAFLDis
regarded to have much atherogenic condition and so cARGHies potential
high cardiovascular risk [5-6]. Early detection of atherogenesis and the
cardiovascular risk related to NAFLD has not been widely researched
[7-8]. In this case-control study, we investigated the relation of NAFLD
with atherosclerosis by measuring carotid intima-media thickness (IMT)
and plaque to detect increased cardiovascular risk.
Materials and Methods
Subjects
We examined all subjects addressed for diagnostic
abdominal ultrasound to the Radiology Division of Bursa High-
Speciality, Education and Research Hospital for fatty liver. 64
patients and 64 sex-and age matched control subjects who
fulfilled the inclusion criteria were participated in the study
after signed informed consent. Complete medical history was
taken and physical examination, anthropometric and laboratory
assessments were performed. Exclusion criteria included: alcohol
consumption of >20 g/day, pregnancy, positive tests indicating
the presence of hepatitis B or C virus, autoimmune liver disease,
hemochromatosis, Wilson’s disease, α-1 antitrypsin deficiency,
primary biliary cirrhosis, primary sclerosing cholangitis and
toxic liver disease.
Clinical and laboratory studies
The diagnosis of NAFLD was established by the exclusion
of common etiologic factors of liver disease and on ultrasound
scanning [9]. Antropometric, complete blood count and
biochemical evaluations were performed. Biochemical
assessments included alanine aminotransferase (ALT), aspartate
aminotransferase (AST), γ-glutamyltransferase (GGT), alkaline
phosphatase (ALP), bilirubin, albumin, total cholesterol, high
density lipoprotein-cholesterol (HDL-cholesterol), triglycerides,
ferritin, C-reactive protein (CRP), fasting glucose, insulin and
c-peptide levels, an oral glucose tolerance test (OGTT). Carotid
ultrasound scanning for determination of IMT and plaque was
performed.Low-density lipoprotein (LDL) cholesterol was
calculated according to the Friedewald formula. Increase in
CRP values accepted when above 3,5 mg/dL. Normal ferritin
levels were between 28-365 mg/mL in men and 5-148 ng/ml
in women. Anthropometric parameters were height, weight,
body mass index (BMI), waist and hip circumferences and
waist/hip ratio values. Appraisement of obesity was dependent
on WHO and NCEP ATP III criteria [10-11]. Definitions of
type 2 diabetes, impaired glucose intolerance were depended
on American Diabetes Association (ADA) criteria. Patients
under oral antidiabetics or insulin therapy were accepted
as diabetics. Hypertension was assumed to be present when
resting blood pressure was ≥140/90 mm Hg or patients were
receiving antihypertensive drug therapy.The homeostasis model
assessment of IR (HOMA-IR) method was utilized to establish insülin resistance (IR) [12]. Patients were accepted as ‘insulin
resistant’ when HOMA-IR value was >2.70.
Liver biopsy was not performed for ethical reasons.
Ultrasound examination is most extensively aplicable method
to diagnose NAFLD. The diagnosis of metabolic syndrome was
set up according to National Cholesterol Education Program
(NCEP) Adult Treatment Panel III (ATP-III) and WHO criteria
[10-11]. Patients should have at least three of the criteria to be
diagnosed with metabolic syndrome. The study was approved by
the hospital ethics committee.
Carotid ultrasound
A Philips HD 11 XE- L12-3 and L12-5 equipment with a
9-MHz multi frequency transducer was used for B-mode and
Doppler carotid ultrasound. Aradio diagnostics and sonography specialist who was unaware of the patients’ and control subjects’
circumstances scanned the right and left carotid arteries
and recorded images on videotape. In the present study İMT
measurements were cARGHied out from the far wall of the distal 10
mm of left and right common carotid arteries. IMT values were
evaluated according to protocols of standard measurements
of carotid artery [13-14]. Increased IMT was defined as a focal
thickening of 1.0 mm in any of 12 carotid segments. A plaque was
defined as a focal thickening above of 1.2 mm in any of carotid
artery segments.
Statistical analyses
Comparisons of patients and control subjects were made with
unpaired t tests or the Mann–Whitney U test, when appropriate,
for continuous variables and by 2 analyses for categorical
variables. Pearson’s correlation coefficients were constructed
to test the relationship between continuous variables. ANOVA
statistic was used to compare sex- and age-adjusted IMT
values between different groups of NAFLD and MetS. P values
<0.05 were considered as statitically significant. Analyses were
performed with SPSS 10.0 software.
Results
Anthropometric, clinical features and laboratory results
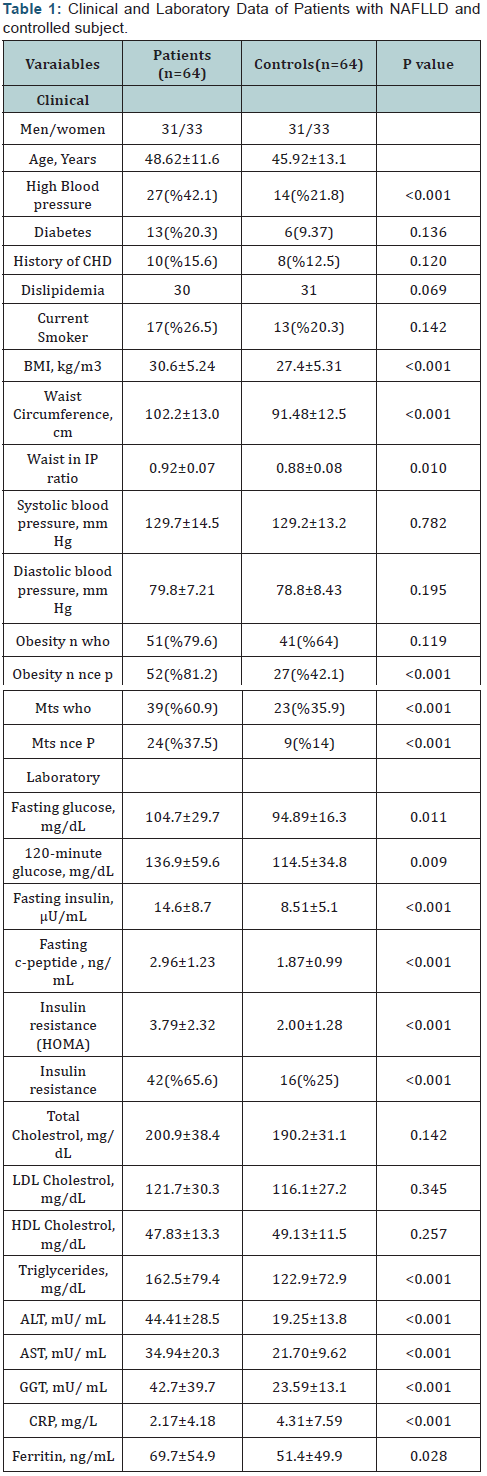
Sixty four patients (31 male, 33 female) and sixty four
control subjects (31 male and 34 female) who were diagnosed
with fatty liver by ultrasonographic examination participated in
the study. Antropometrical, clinical features and laboratory data
in both group were compared and shown at (Table 1). Patients
with NAFLD had a higher frequency of high blood pressure than
control group as statistically. Only ten patients with NAFLD had
a history of CHD and there was no significant difference when
compared to those in control group. BMI and central obesity
measures were higher significantly in NAFLD group than in
control subjects.
Fasting and 120-minute glucose values were higher
in patients with NAFLD than those in control indivudials and
were not significant (Table 1). Fournew cases of diabetes among
NALFD patients and threecases in control subjects were detected
by OGGT. Fasting insulin, fasting c-peptid and HOMA-IR values
were significantly higher in NAFLD patients. Herewith, NAFLD
patients had high frequences of insulin resistancy significantly.
Total cholesterol, LDL cholesterol and HDL cholesterol levels
were similar in two groups, but in NAFLD group triglycerides were higher than those in controls. The levels of serum alanine
aminotransferase (ALT), aspartate aminotransferase (AST) and
γ-glutamyl transpeptidase (GGT) were higher in NAFLD patients
significantly.Interestingly a high ferritin level was present only in
one female NAFLD patient and was not detected in control group.
This patient had metablic syndrome and was insulin resistant,
but IMT values werein normal ranges.
Unexpectedly, in the present study, CRP levels were
higher in control group than those in NAFLD patients. Elevated
serum CRP was present in 6 (6,25%) of NAFLD patients and 19
(23,4%) of control subjects (P<0.001). For all that, interestingly,
control group with high CRP values had increased IMT and
plaque formation significantly.
Findings due to metabolic syndrome
Three metabolic risk factors related to MetS (obesityincreased
BMI, central obesity, hypertension, insulin resistance)
were significantly(P<0,001) more frequent in NAFLD patients
than those in control subjects. But the frequency of diabetes and
dislipidemia were similar in both NAFLD and control groups. As
to both WHO and ATP-III criteria,the frequency of MetS in NAFLD
patients was higher than normal subjects.(60,9% and 37,5%
versus 35,9%and 14% respectively). According to the presence
of metabolic syndrome, in NAFLD group plaque formation was
higher than control group (Table 2).
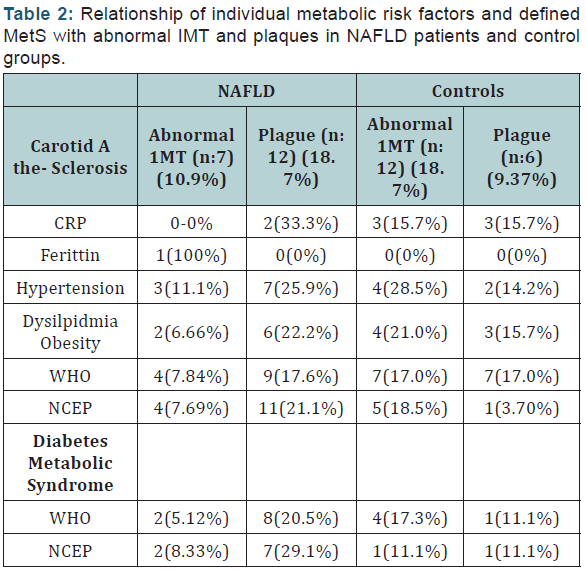
Outcomes of carotid ultrasound examinations
Aimed to present the predictors inducing the occurance of
carotid atherosclerosis in NAFLD patients comparing to control
group (Table 2). At the same time, the abnormal IMT rates and
plaque formation according to the presence of metabolic risk
factors in NAFLD patients and control group were shown at
(Table 2) and no risk factor seemed to be as the predictor of
carotid atherosclerosis.
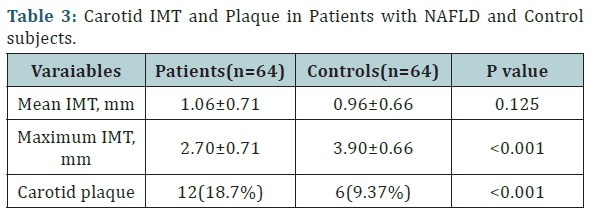
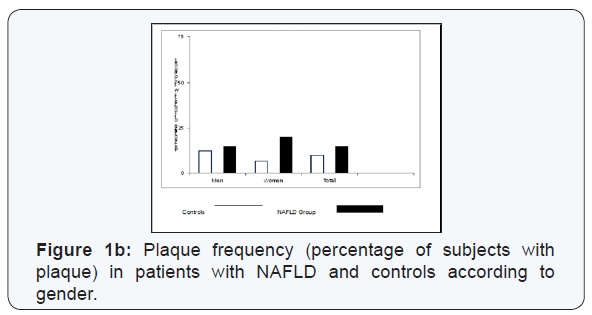
Patients with NAFLD showed increased mean IMT and a
2-fold higher frequency of plaque comparing to normal subjects,
but conversely maximum IMT value was higher in normal group
than those in patients with NAFLD (Table 3). The differences
for mean IMT between NAFLD and controls were 0.10 mm in
favour of NAFLD group and 1.1 mm for maximum IMT in favour
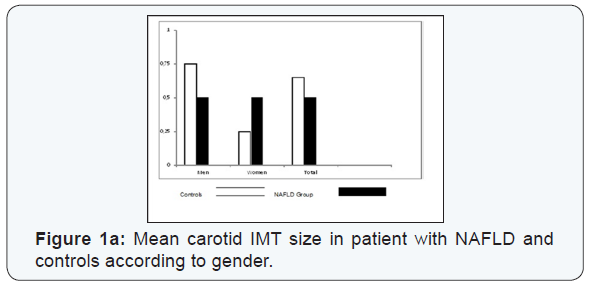
of healthy controls. Figure 1 shows patient-control differences
in IMT and plaque frequency according to the gender. In NAFLD
group IMT values were higher in women than those in men.
Conversely, in control group IMT values were higher in men than
those in women.
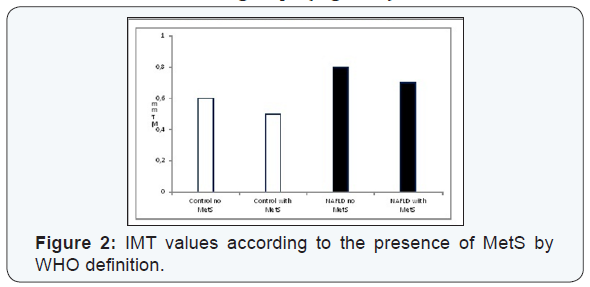
When we compared all participants subdividing into 4
subgroups as with andwithout NAFLD and with and without
MetS, IMT values did not show significant differences and were
almost similar in four subgroups (Figure 2).
Discussion
This study aimed to evaluate the coexistance and size of
cardiovascular risk factors and carotid atherosclerosis in patients
with primary NAFLD diagnosed by ultrasound examination. As to
recent studies, patients with NAFLD frequently presents various
combinations of parameters related to MetS [3-4]. While MetS
has high risk of atherosclerosis and is associated with NAFLD,
studies to determinate early atherosclerosis and detection of
novel atherosclerotic risk factors in NAFLD patients were widely
studied recently as stated by Targher G et al. [5]& Lim S et al. [6].
In this study, the prevalance presence of carotid
atherosclerosis was investigated in patients with NAFLD being
coexistence with or without metabolic syndrome. Carotid
atherosclerosis has a significant value to predict the oncoming
atherosclerotic process. Stated that values of carotid intimamedia
thickness were reliable and accurate method to detect
early athrerosclerosis [7-8]. Various methods are available
for measurements of carotid aretry intima-media thickness as
showed by Casella IB and BaldassARGHe D [13-14]. NAFLD and the
progress of an atherosclerosis now a rising issue in the field of
cardiovscular risk factors as stated by Brea A et al. [14],Volzke H
et al. [15] Nestel PJ et al. [16].
In the present study, abnormal IMT and carotid plaque
incidence, as the signs of developing atherosclerosis, were
not associated with MetS and its individual parameters in
patients with NAFLD and in controls (Table 2). According to
the literature, in subjects with MetS, incidence and progression
of augmented carotid IMT and carotid plaque occurance were
increased Kim HC et al, Targher G et al & Bonora et al. [18-20]
said that presence of Mets in NAFLD cases enhances occurance
of carotid atherosclerosis [18-20]. In this study in NAFLD group
with WHO-MetS had an increase in plaque formation than those
in controls but this result was not significant. Regardless of
MetS, in NAFLD and control groups have similar ratio according
to the presence of increased IMT and carotid plaque formation
and these findings suggest that, solely NAFLD did not increase
the occurance of atherosclerosis (Table 3). Kim HJ et al and
Younossi Zobair M et al. [21-22] said that NAFLD could occur in
adolescents and in leans even in the absence of MetS [21-22],
likewise, carotid atherogenesis might progress even so in healty
and young persons [23-27]. These findings give hints that NAFLD
is not always and un questionable an atherogenic state. Large
numbers of individuals with and without NAFLD as well as with
and without MetS should be studied for carotid atherosclerosis.
Prevalence of MetS in our NAFLD and control groups were
60,9% and 35,9% respectively and results were statistically
significant. But in the present study NAFLD did not have close
relation with increased IMT and carotid plaque. The presence
of MetS did not change the outcomes. Presence of MetS did not
alter the generation of abnormal IMT and carotid plaque and
these findings were not concordant with the view of NAFLD as a hepatic component of MetS [28]. Additionally, hepatic fat
accumulation was not significantly related to patients’ lipid
profile, atherogenic condition.
Howbeit, conversely to certain previous study findings, in the
present study we determined that patients with NAFLD might
not have advanced carotid atherosclerosis and NAFLD could not
be a predictor of an increased IMT [23-25]. Targher G et al, Petit
JM et al and Oren A et al revealed that carotid arteriosclerosis
could be present in young and healty adults.
Process of atherogenesis in NAFLD can be revealed by
measuring CRP levels [29]. In the pathogenesis of NAFLD
oxydative stress has an importanat role. Pro-atherogenic effect
in NAFLD is considered to become from exessive oxydative
stress. Alongside being the source of oxydative stress, ROS
(reactive oxydative species) eventuate from fatty acid betaoxydation
and cause hepatocyt injury, cytokin release and
yield an inflammatory milieu which can initiate also steatosis
and steatohepatitis and then additionally an atherognic effect
together with the increased level of serum CRP. In our study CRP
levels were higher in control group than those in NAFLD subjects,
despite the presence of MetS. In the present study CRP levels
were not increased in insülin resistant individuals. Moreover,
CRP levels were not related to the serum ALT levels and IMT
values. So CRP and ALT both did not show any association with
the inflammatory state.
Additionally, abnormal lipoprotein metabolism (due to
the insulin resistance and MetS) in NAFLD can enhance the
cardiovascular risk and effect the formation of atherosclerosis
[30]. A considerable and common mechanism of hepatosteatosis
is as belows: increased fatty acid flow from adipose tissue and
small intestine because of the removed inhibition of lipoprotein
lipase enzyme effect on lipolyse secondary to insulin resistance,
reduced beta-oxydation and increaed synthesis of free fatty acids
in hepatocytes and reduced triglyceride excretion from liver cells.
The latest depends on the deteriorated synthesis of Apo-B100
and diminished formation of VLDL. Because of the reducing
hepatic Apo B synthesis in NAFLD, triglyceride rich VLDL is not
excreted and accumulates in liver. Increased intracellular free
fatty acids cause an enhancement of cytochrome P450 4A and
cytochrome P 2E1. These products then induce the occurance
of ROS. Excessive ROS initiate lipid peroxydation of hepatocyte
membrane lipids and then destruction of liver cells emerges
[31]. In the present study, in NAFLD patients and controls with
dyslipidemia, percentages of those with abnormal IMT and
carotid plaque were similar and results were not significant.
Whereas, serum triglyceride levels were increased in NAFLD
patients than those in control subjects significantly.
Free radicals are occured also during the enzymatic and
non-enzymatic oxydoreduction reactions concerned with iron
and copper [32]. Free radicals break up double bonds between
carbon atoms in unsaturated fatty acids with the catalytic effect of iron and ascorbic acid. The result is the onset of lipid
peroxydation. Ferritin is the form of iron storage, and iron
is released to provide the necessaty of the body. The role of
excessive iron storage is not exactly clear in pathogenesis of
NAFLD. In NAFLD, because of being an acute phase reactant
ferritin may be increased secondary to the inflammation and
liver cell damage. In this study, only one patient had high ferritin
level. This female NAFLD patient was obese and insulin resistant
and had hypertension with normal ALT levels. In both groups
ferritin levels were also not correlated with increased IMT values
and presence of plaque.
In conclusion, in our study NAFLD was not associated with
carotid atherosclerosis or atherogenetic state even with and
without MetS. While NAFLD is considered as a component of
MetS, the findings and results of our study maydirect attentions
to other causes which lead to the formation of atherosclerosis.
The frequency of CAD, components of MetS or defined MetS may
show disparity in NAFLD according to the recent studies. Howbeit,
in NAFLD patients with or without MetS, should be evaluated for
an unknown and ocult and potential cardiovasculsar risk as well
as a serious liver disease.
For more articles in Advanced Research in Gastroenterology &
Hepatology
Journal click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment