A Case of Successful Use of Biliary Duct Balloon Dilator in Repairing Postsurgical Esophageal Stricture in an Infant at the Age of 3 Months
Authored by Deepankar Kumar Basak
Abstract
Esophageal atresia is an abnormality, or birth defect
of the esophagus that occur early in pregnancy. One or more fistula may
be present between the malformed esophagus and trachea. The lack of
esophageal patency prevents swallowing. Congenital Esophageal Atresia
(EA) needs to be surgically corrected as soon as possible. Some will
present with post surgical stricture that needs to be dilated by a
balloon dilator. This procedure is difficult in premature born due to
infant esophageal size and availability of equipments. We hereby report
the first case in a premature infant with post surgical esophageal
stricture of esophageal atresia by the use of biliary duct balloon
dilator.
Keywords: Balloon dilator; Esophagus; StrictureIntroduction
The most common gastrointestinal atresia is
congenital esophageal atresia (EA). Blind proximal esophagus with
fistula between distal esophagus and the Tracheoesophageal Fistula (TEF)
is the most common type. Treatment is by extra pleural surgical repair
of the esophageal atresia and closure of the tracheoesophageal fistula.
Development of post-surgical esophageal stricture is a common
complication. These anastomotic strictures can cause dysphagia, feeding
difficulties, feeding tubes (nasogastric or gastrostomy) dependency. For
partial strictures conservative endoscopic management is preferred [1].
A major limiting factor to this approach is the esophageal abnormal
anatomy and motility. Endoscopic dilatation can be performed
successfully with over guide wire ante grade dilation using Savary-
Gilliard bougies1 or under direct visualization using cre balloon
dilatation under fluoroscopic guidance [2]. Sever anastomotic stricture
may not be traversed with a standard guide wire, for that a retrograde
gastric endoscopy can be considered. This approach has been associated
with many complications (infection, bleeding and formation of fistula)
especially in patients who require gastrostomy tube placement for this
retrograde approach [3]. The use of biliary type guidewire in dilating
strictures that are not traversable endoscopically has been reported
[4]. The use of biliary-type guidewire in dilating sever anastomotic
esophageal stricture post-surgical TEF repair has not been described in
our country. We describe a safe, successful and feasible technique to
dilate sever esophageal stricture in a three month- old male infant that
was otherwise inaccessible by a standard antegrade endoscopic
approaches.
Case Report
A 3 months baby named Awsaf weighting 2.5 kg was born
at 37 weeks of gestation by normal vaginal delivery. Just after
delivery, baby was tried for breast feeding but regurgitation of milk
occurs through mouth and nose. Then baby was admitted to hospital. By
doing USG and barium swallow, it was found that boy had the most common
variant of EA and TEF which was 3 mm from the tracheal wall. Prenatal
sonogram was failed to show the most common variant of EA with TEF due
to lack of good trained sonologist. After 25 days, surgery was performed
to correct TEF
(right posterolateral 4th intercostals, transpleural thoracotomy
with ligation of distal trachea esophageal fistula and end to
end esophageal anastomosis was done) [5]. Post operative
nasogastric feeding was started from 2nd day on wards. After one
moth boy again developed regurgitation, after barium swallow
it was found to develop stricture at the anastomotic site. Then
patient was referred to Gastroenterologist for upper endoscopy
and likely balloon dilation of his anastigmatic stricture that was
seen on a barium study. The presumption was that the esophagus
would have nARGHowing around the anastomosis area [6].
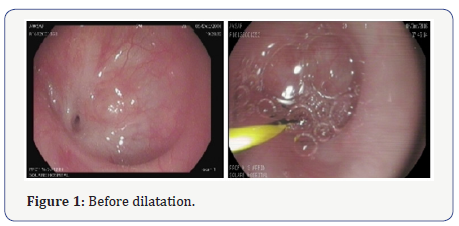
After doing endoscopy, tight nARGHowing of the esophagus is
noted at 10 cm from the incisor teeth (about 5 cm from the upper
esophageal sphincter) (Figure 1). Initially dilatation was tried by
Savary Gilliard dilator up to size 5 mm but dilatation was not
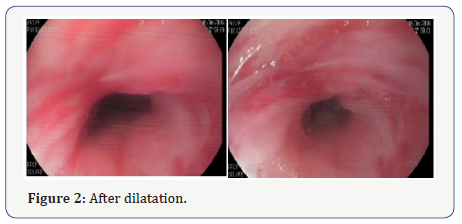
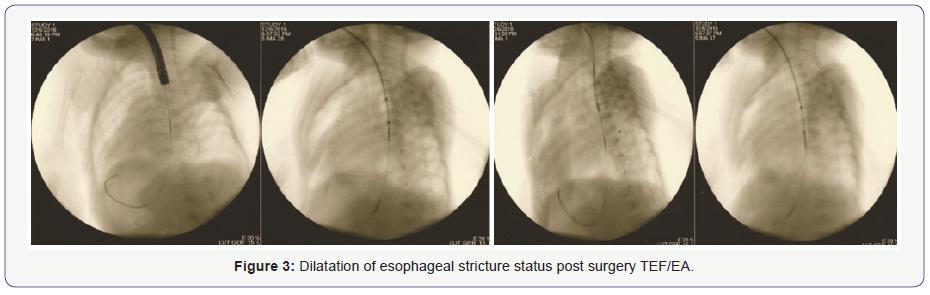
successful. Ultimately dilatation is done by hurricane balloon
dilator under fluoroscopic control. Repeat endoscopy confirms
adequate dilatation and allowed the scope to pass easily (Figure
2&3). Lower esophageal sphincter is at 15 cm from the incisor
teeth.
Discussion
Endoscopic management of postsurgical esophageal
strictures is usually sufficient and successful, few cases of
sever strictures or complete obstruction may need surgical
interventions. In these cases the use of Biliary Balloon dilators
can be the solution, before sending them for invasive surgical
options like gastric or colonic interposition. Our case with a
primary esophageal atresia repair complicated by subsequent
anastomotic stenosis that underwent a successful procedure
by using Biliary duct balloon dilator to dilate the esophageal
lumen. The long-term patency and success of this procedure in
this individual patient will need to be further evaluated with
follow-up studies as clinically indicated. To our knowledge,
there is no other case documented in the literature of an
attempted esophageal dilatation using the biliary balloon before
in our country). Inserting the wire under direct visualization
through the scope confirms in the stomach decreases the risk
of wire placement related perforation under fluoroscopy. After
confirming the wire placement, biliary balloon dilators can
be used in this setting to dilate sever esophageal strictures
successfully. The use of endoscopic biliary accessories in dilating
sever esophageal strictures should be considered before sending
these patients to invasive retrograde gastroscopy dilation or
surgical interventions.
Conclusions and Recommendations
The use of biliary baloon dilators is safe and feasible in
managing tight non traversable esophageal strictures (< 6 mm).
This technique should be considered before sending all patients
for more surgical portion
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment