Clinical and Laboratory Study on Children with Glycogen Storage Disease Type-1 in Upper Egypt
Abstract
Background: One of the GSDs that
principally affect the liver is Type 1 GSD. GSDI patients may present
with fast-induced hypoglycemia and hyperlactacidemia. More commonly, the
first symptom is the presence of a protruded abdomen due to marked
hepatomegaly.
Study aims: This study aims to
assess frequency, clinical manifestations, biochemical features of GSD1
in children attending University Hospitals in Upper Egypt, and to
identify the possible role of plasma biotinidase in diagnosis of GSD-1
in these children.
Patients and Methods: Any child
with unexplained hepatomegaly with growth retardation, early fasting
hypoglycemia, hyperuricemia, or hyperlipidemia during the period from
July 1st 2011 up to December 31st 2013 was included in this study.
Complete blood counts, liver function tests, Prothrombin time and
concentration, serum glucose, cholesterol, triacylglycerol, plasma
biotinidase, Plasma lactate and plasma uric acid level were measured.
Liver biopsy was done to patients when needed and Glucose-6-phosphatase
activity was measured in biopsied liver tissue.
Results: GSD-1 could be detected in
only 10 children. 50% of them males and 50% females, with the mean age
4.8+4 SD years, 8(70%) between 1 to 6 years old. The histopathological
diagnosis of GSD-I was confirmed. There was lower glucose-6-phosphatase
activity in the biopsied liver tissue homogenates and high plasma
biotinidase was detected in these 10 children.
Conclusion: GSD-1 should be
considered in all children with unexplained hepatomegaly. Elevated serum
biotinidase can be used as a diagnostic marker for hepatic glycogen
storage disorders and Biotin supplementation in children with GSD-1 is
very important.
Keywords: Type 1 GSD; Children
Abbreviations: PPV: Positive
Predictive Value; NPV: Negative Predictive Value; GSD: Glycogen Storage
Disease; SPSS: Statistical Science for Social Package
Introduction
Because liver has central role in synthetic,
degradative and regulatory pathways involving carbohydrate, protein,
lipid, trace elements and vitamin metabolism many metabolic
abnormalities affect the liver [1]. One of the inherited metabolic
disorders that principally affect the liver is Glycogen storage disease
Type 1 (GSD-1), which is caused by the absence or deficiency of glucose-
6- phosphatase activity in the liver this leads to inadequate
conversion of the glucose - 6- phosphate to glucose and makes affected
individuals susceptible to fasting hypoglycemia [2]. GSD-I patients may
present with fast-induced hypoglycemia (sometimes occurring rapidly in
about 2 to 2 and a half hours after a meal) and hyperlactacidemia in the
neonatal period. More commonly, the first symptom is the presence of a
protruded abdomen due to marked hepatomegaly around 3 months of age,
though in some cases the liver may already be enlarged at birth.
Fasting tolerance is very limited: hypoglycemia, which may cause
convulsions, and lactic academia, account for the initial gravity
of the disease [3,4]. Early diagnosis and treatment is important
for improving quality of life, reducing the damaging effects on
organs that become engorged with glycogen, and extending
the patient’s life span [5]. Clinical and laboratory evidence
often guide the evaluation. Liver biopsy offers morphologic
study and permits enzyme assay. Genetic diagnostic approach
also available [1]. Biotinidase, the biotin recycling enzyme is
ubiquitously distributed and occurs at high levels in the liver,
serum, and kidney. It is synthesized by the liver and secreted
into the blood [6]. An increase in glucose-6-P or lactate act as
activators for biotinidase and this is the cause of the observed
increase of biotinidase in plasma of patients with GSD-1. This
suggests the possibility of diagnosis or at least strong support
for the diagnosis of GSD-1 and liver biopsy may be avoided
[6,7]. Aim of the work: This study aims to assess frequency,
clinical manifestations, biochemical features of GSD-1 in
children attending Assiut University children Hospital, pediatric
departments of Sohag and Qena university hospitals, Upper
Egypt and to identify the possible role of plasma biotinidase as a
rapid non invasive and conventional biochemical marker in the
blood for diagnosis of GSD-1 in these children.
Patients and Methods
This cross sectional, hospital based study was cARGHied
out from July 1st 2011 up to December 31st 2013 in Assiut
University children Hospital, pediatric departments of Sohag
and Qena university hospitals, Upper Egypt. This study was
approved by the Ethical Committee of Faculty of Medicine, Assiut
University, according to the latest revision of Declaration of
Helsinki and informed consent was obtained from participant’s
parent/legal guardian. The inclusion criteria of this study were
any child with hepatomegaly with clinical suspicion of having
a metabolic disorder e.g. growth retardation, failure to thrive,
dimorphic features or seizures. Children with proven infectious,
hematologic, toxic, autoimmune or even malignant cause of
hepatomegaly were excluded from this study. During the study
period all children with the inclusion criteria were included in
this study, they were 40 children (25 male and 15 female). Full
clinical assessment was performed to all patients including
thorough history and clinical examination. All children included
in this study were subjected to the following: abdominal
ultrasonography, complete blood counts, liver function tests,
Prothrombin time and concentration, serum glucose, plasma
cholesterol, plasma triacylglycerol, plasma lactate, plasma uric
acid level. Plasma biotinidase level was measured by using
enzyme-linked immune-sorbent assay (ELISA) multiskan EX
micro plate photometer, thermo scientific, STAT FAX-2100,
USA(Glory Science Co., Ltd, CATALOG #: 95562, USA). Under
sonographic guided percutaneous needle liver biopsy were
done to patients when needed: Variable liver tissue cores
ranging from 0.3 to 2 cm in length were taken from the pediatric
patients using spring loaded biopsy needle “18G Х 16 cm” GTA, LP 0019\12-Italy. Part of the biopsy core was embedded in 10%
formalin for histopathological examination using Hematoxylin
& Eosin “H&E” stain. Diagnosis of glycogen storage disease
based on the presence of mosaic pattern of the hepatocytes
with the presence of periodic acid-Schiff staining “PAS” positivediastase
sensitive inclusions which are glycogen deposits in liver
biopsies of these children [8]. Glucose-6-phosphatase activity
was measured in biopsied liver tissue homogenates according
to Koide & Oda [9] and King [10] and total proteins Spectrum
Diagnostics total protein reagent “Biuret reagent”(CATALOG #:
310 001, Germany) have been measured in the homogenate using
T60 UV visible spectrophotometer. Then the enzyme activity in
units was divided by the total protein per mg tissue to give the
enzyme activity in units/mg tissue protein.
Statistical Analysis
Statistical Science for Social Package (SPSS V12, SPSS Inc.,
Chicago, IL, USA) was used for data analysis. Data were presented
as mean (SD) or number (%) as appropriate. For comparison of
two groups, the parametric ‘Student’s t test’ and non-parametric
‘chi squared test’ for independent variables were used. For all
tests, a probability (p) <0.05 was considered significant. To
detect if the serum biotinidase can be used as diagnostic marker
in children with GSD-1, Sensitivity (ability of the test to detect
+ve cases), Specificity (ability of the test to exclude negative
cases), positive predictive value (PPV) and negative predictive
value (NPV) were calculated.
Results
Among the 40 children included in this study GSD-1 could
be detected in only 10 children. They were 5 (50%) males and 5
(50%) females, with the mean age 4.8+4 SD years and age range
0.025-16 years. The histopathological diagnosis of GSD-I was
confirmed in all these 10 children. This based on the presence
of mosaic pattern of the hepatocytes with the presence of
periodic acid-Schiff staining “PAS” positive- diastase sensitive
inclusions which are glycogen deposits in liver biopsies of these
children [11]. The main histopathological findings of the GSD-I
patients involved in this study were in the form of fatty changes,
nuclear hyperglycogenation and fibrosis. They were graded 0-3
according to Gogus et al. [11]. All GSD-1 patients showed fatty
changes and nuclear hyperglycogenation in varying degrees from
grade 1 to grade 3 but as regard the degree of fibrosis, two cases
show no fibrosis (grade 0), one case showed massive fibrosis
merging to cirrhosis (grade 3) and the remaining cases showed
mild to moderate fibrosis in varying degrees from grade 1 to
grade 2. There was also, lower glucose-6-phosphatase activity
in the biopsied liver tissue homogenates of these 10 children.
According to clinical, laboratory and histopathological findings,
all children included in this study were divided into two groups:
- Group A: contains 10 pediatric patients with the provisional and final diagnosis of glycogen storage disease GSD- 1.
- Group B: contains 30 children with the provisional diagnosis of glycogen storage disease according to the inclusion criteria but the final diagnosis wasn’t glycogen storage disease.
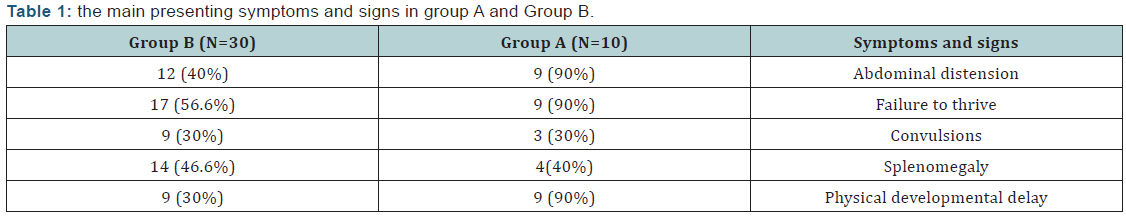
(Table 1) shows the main presenting symptoms and signs in
group A and Group B.
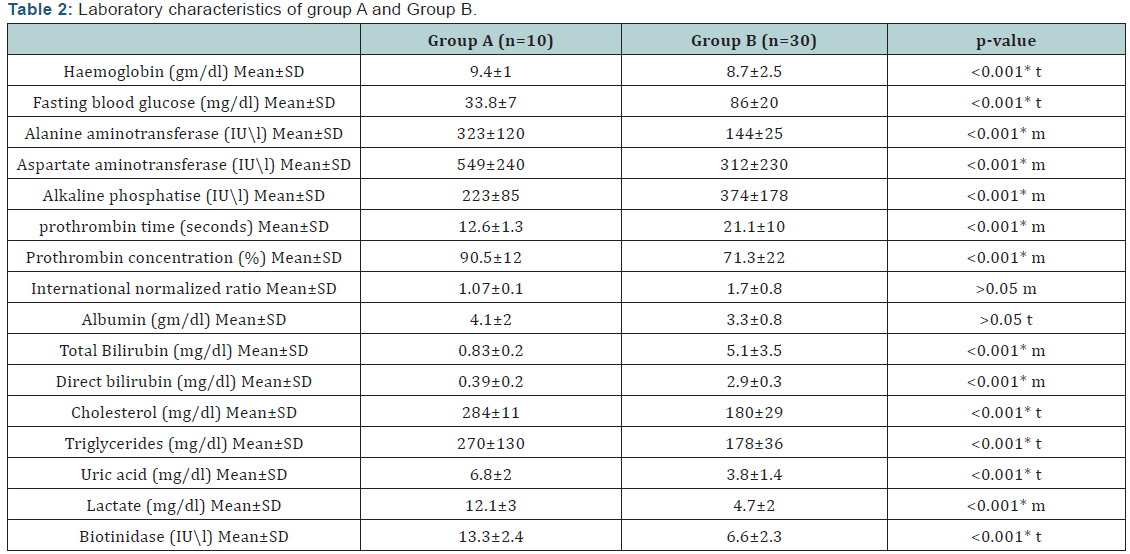
(Table 2) shows Laboratory characteristics of group A and
Group B.
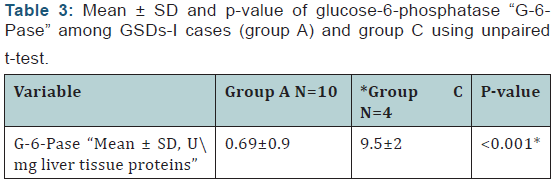
(Table 3) shows comparison between of glucose-6-
phosphatase “G-6-Pase” among GSDs-I cases (group A) and
control group.
The results of this study show that plasma biotinidase has
positive predictive value 80%, negative predictive value 95%,
sensitivity 91% and specificity 74% in GSD-I patients.
Discussion
Based on clinical, biochemical and histopathological findings
10 children proved to have GSD-I in this study. They were 5 males
& 5 females with no statistically significant difference regarding
sex. In agreement with these findings, previous studies [12,13]
reported that the sex ratio among the studied GSD-I patients
was 1:1. Regarding the clinical presentation in the present
study, abdominal distension, failure to thrive and physical
developmental delay were present in 90% of GSD-I patients,
convulsions were present in 30% of them and hepatomegaly was
present in all GSD-I patients (100%). This is in accordance with
previous studies [13-16] who reported that the main complaint
in GSD-1 patients was abdominal protruding with different rate
from 57.8%- 83.3% of cases, followed by growth retardation in
40%- 50% of cases and hepatomegaly was present in 100% of
cases. The main laboratory findings of GSD-I patients involved in
this study, fasting hypoglycaemia and anemia, have the highest frequency (100%), followed hyperlipidemia (80%) followed
by hyperuricemia (70%), while hyperbilirubinemia has the
lowest frequency (30%). In agreement with these findings,
previous studies [14,16,17] reported that hypoglycemia,
hypertriglyceridemia, lactic acidosis, hyperuricemia were the
most frequent laboratory findings among GSD-I patients. Also
Carvalho et al. [18] found that all patients with GSD-1 in their
study had anemia.
Among GSD-I patients in this study, there were statistically
significant raised transaminase. These results differ from what
reported by Priya et al. [2] who stated that despite marked
hepatomegaly, the liver transaminase levels are usually normal
or only slightly elevated. But in accordance with the results of
other studies [14,16] who found that there was a consistent
increase of amino transferases in serum among GSD-1 patients
involved in their studies. Glycogen storage leads to hepatocytes
injury with subsequent elevation of liver transaminase [19].
In the present study, the plasma biotinidase activity in
patients with GSD-I showed statistically significant increase
versus the other group. Also the results of this study revealed that
plasma biotinidase is considered better positive than negative in
prediction of GSD-I with higher sensitivity and low false negative
rate. In agreement with these findings, the results of previous
studies [15,20,21] who reported that markedly elevated serum
biotinidase were found in cases of GSD-1, concluding that GSD-1
should be considered in children with elevated serum biotinidase
activity. Also, Paesold Burda et al. [22] proposed from the results
of their study that elevated serum biotinidase can be used as a
diagnostic marker for hepatic glycogen storage disorders.
Regarding the liver biopsy, the histopathological diagnosis
of GSD-1 was confirmed in all 10 children involved in group 1.
This based on the presence of mosaic pattern of the hepatocytes
with the presence of periodic acid-Schiff staining “PAS” positivediastase
sensitive inclusions which are glycogen deposits in liver
biopsies of these children8. The main histopathological findings
of the GSD-1 patients involved in this study were in the form of
fatty changes, nuclear hyperglycogenation and fibrosis. They
were graded 0-3 according to Gogus et al. [11]. All GSD-1 patients
showed fatty changes and nuclear hyperglycogenation in varying
degrees from grade 1 to grade 3 but as regard the degree of fibrosis,
two cases show no fibrosis (grade 0), one case showed massive
fibrosis merging to cirrhosis (grade 3) and the remaining cases
showed mild to moderate fibrosis in varying degrees from grade
1 to grade 2. These findings are in accordance with Saltik et al.
[15] who reported that the histopathological findings of the liver
included fibrosis (75.6%), steatosis (37.8%), mosaicism (24.4%)
and nuclear hyperglycogenation (15.6%) among GSD-I involved
in his study. There was also, highly statistically significant lower
glucose-6-phosphatase activity when measured in the biopsied
liver tissue homogenates of the GSD-1 patients when compared
with the control group. This is in accordance of other studies who reported that diagnosis of GSD-1 is suspected on the basis of
clinical and laboratory findings and definitive diagnosis required
liver biopsy and the diagnosis was confirmed by the finding of
very low glucose-6-phosphatase activity [4,17].
Conclusion
GSD-1 should be considered in all children with unexplained
hepatomegaly, with or without hypoglycemia. Orientation of
young mothers about symptoms of GSD-1 to seek early medical
advice is very important. Elevated serum biotinidase can be used
as a diagnostic marker for hepatic glycogen storage disorders.
To Know More About Open
Access Journals Publishers Please Click on: Juniper Publishers



Comments
Post a Comment