Sonographic Evaluation of Liver Cirrhosis: Causes and Pathophysiology _Juniper Publishers
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by M Ayub Hussain
Introduction
Liver cirrhosis existed since ancient times. It is widely speeded all over the world various causes:
a. Known and unknown
b. Signs and symptoms may be different for patients in
Biopsy is not the only and 100% positive test for Liver cirrhosis diagnosing. Clinical history, physical examination, signs and symptoms, blood works and Ultrasound evaluation can diagnose liver cirrhosis most of the time without the need of biopsy. Ultrasound is a helpful modality. Inexpensive, quick, available, noninvasive, portable, repeatable and more over non radiation. Elastography is a kind of ultrasonography recently started commercially.
Goals and Objectives
At the end of this session, we will learn the impact in details about:
a. Patient history
b. Details physical examination
c. Selective blood works
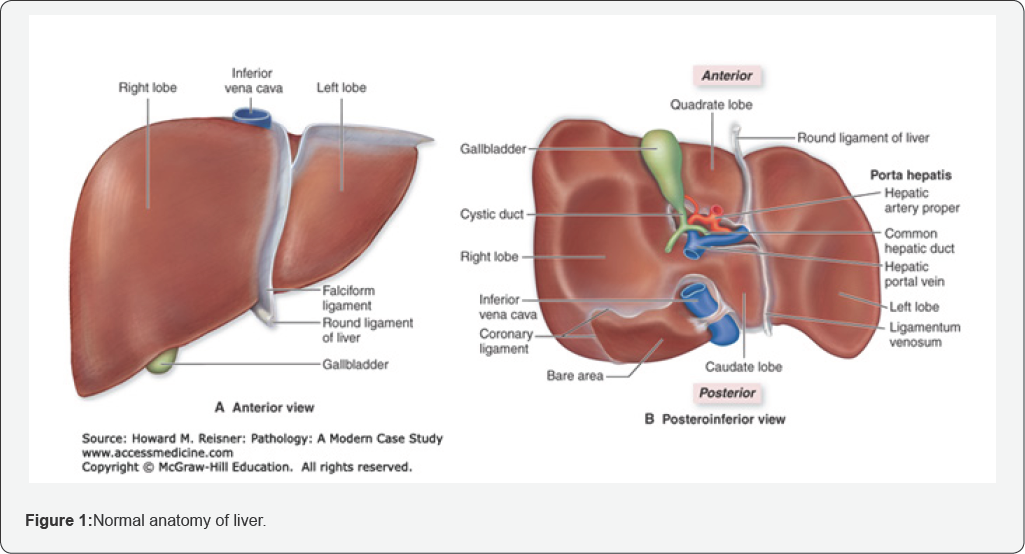
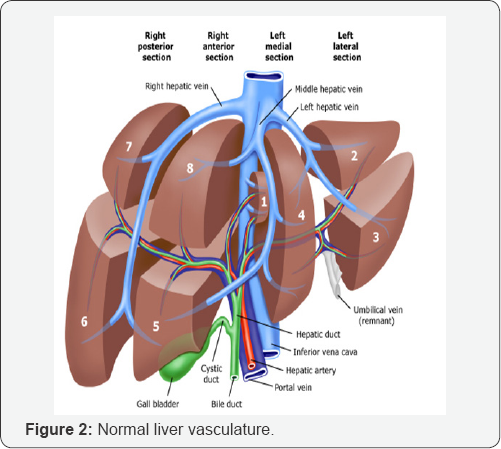
d. Sonography evaluation in order to diagnose the liver cirrhosis without biopsy (Figure 1-5).

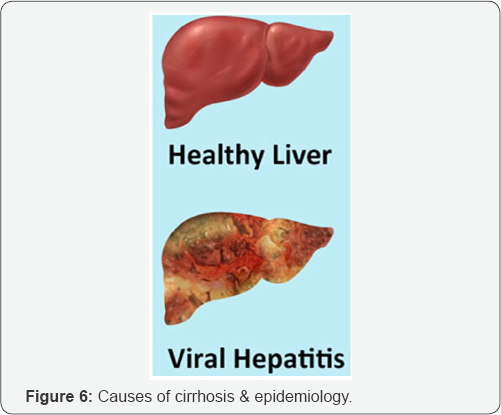
Causes of Cirrhosis & Epidemiology
a. Alcoholic cause is more prevalent in western countries 60-70%.
b. Non Alcoholic viral causes: Hep B and C
c. Higher in developing countries, especially Asia and Africa.
d. Inadequate screening test for blood transfusion and contamination from dialysis machine.
e. Unprotected sexual activity (Figure 6).
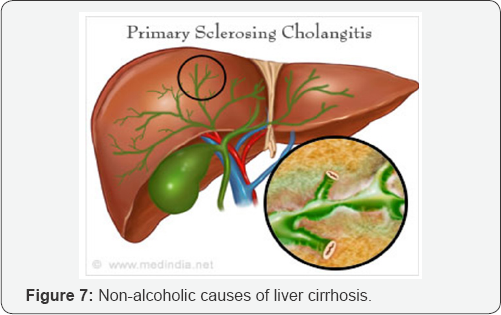
Non-Alcoholic Causes of Liver cirrhosis
a. NASH (Non Alcoholic Steatohepatitis).
b. Metabolic: Haemochromatosis, Wilson's disease, fatty infiltration and Alpha-1 antitrypsin deficiency
c. Auto-Immune hepatitis.
d. Biliary disease: primary sclerosing cholangitis and primary biliary cirrhosis.
e. Vascular disease: congestive hepatopathy, Budd-chiari syndrome and hepatic veno-occlusive disease.
f. Medications: Methotrexate.
g. Cystic fibrosis: uncommon (Figure 7).
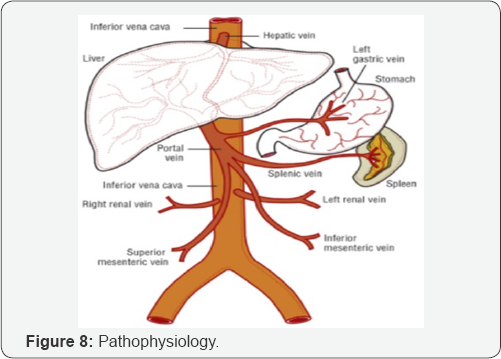
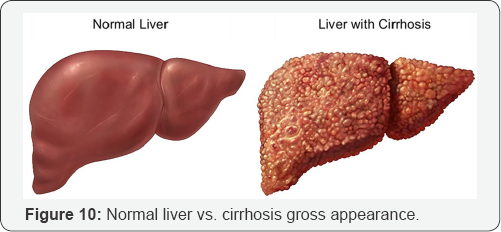
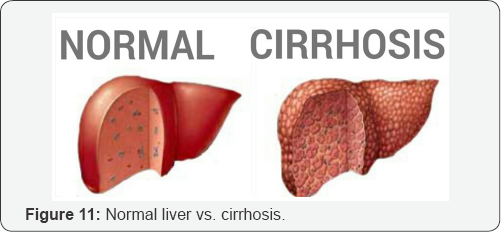
Pathophysiology
Steps
a. Fibrosis.
b. Nodular regeneration.
c. Distortion of liver architecture (Figure 8).
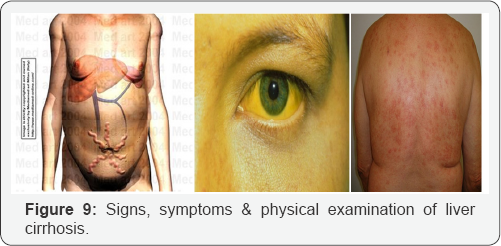
Signs, Symptoms & Physical Examination of Liver Cirrhosis
There’s no typical signs or symptoms of liver cirrhosis because depends on the stages and athophysiology of the disease.
I. Early stage: Asymptomatic
II. Late stage:
a. Malaise
b. Fatigue
c. Lack of appetite
d. Frequent loose motion after eating
e. Distended and heaviness of abdomen
f. Pain in left hypochondriac
g. Muscle wasting
h. Hemorrhoids
i. Dizzy
j. Jaundice
k. Skin itchy
l. Hepatic faces
m. Caput medusa
n. Disorientation: Dementia and amnetia (Figure 9).
Diagnosing Cirrhosis: Blood Works
a. Blood tests to check liver functions: Albumin and Total serum protein.
b. Prothrombin time/INR.
c. Bilirubin
d. Liver enzymes: AST, ALT and lactate dehydrogenase.
e. Alkaline phosphatase.
f. Hepatitis B and Hepatitis C antigen and antibody.
g. Alpha 1-antitrypsin.
h. Blood alcohol test.
i. Antinuclear antibody (ANA), Anti- smooth muscle antibody (ASMA), Anti-mitochondrial antibody (AMA).
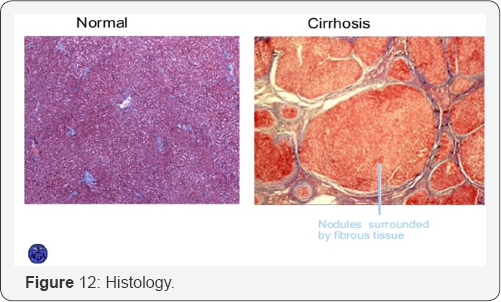
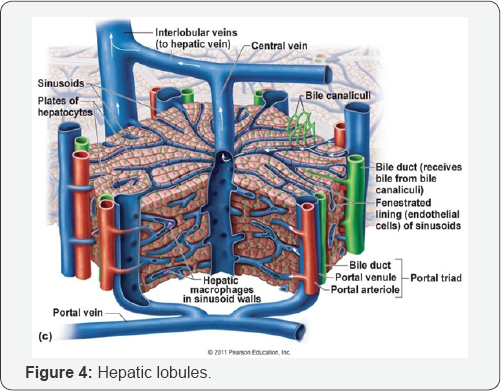
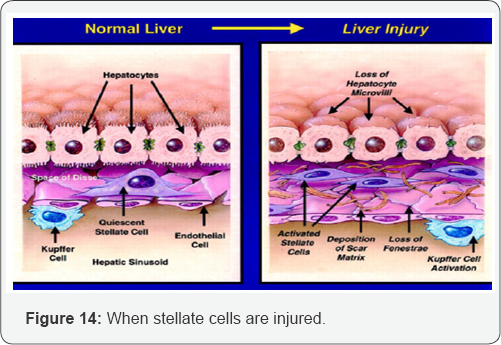
Insult of Liver Cells
A. Stellete cells
a. Fibrin, collagen and intercellular matrix release.
B. Hepatocytes
a. Formation of regenetive nodules.
C. Sinusoid compression
a. Obstruction of blood flow.

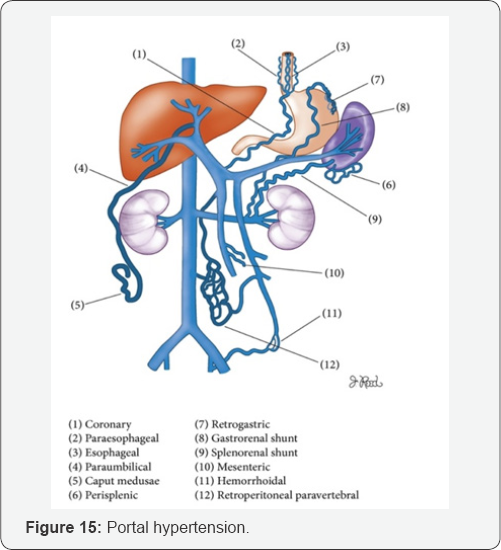

Portal Hypertension
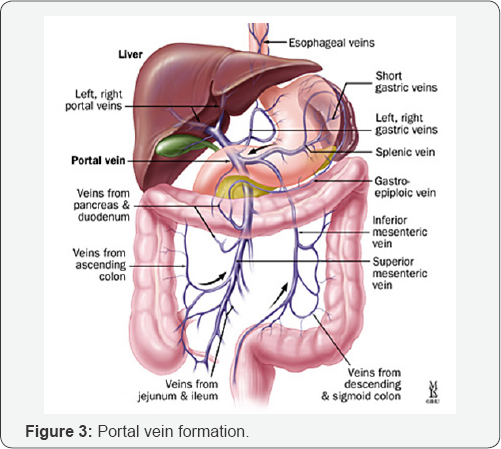
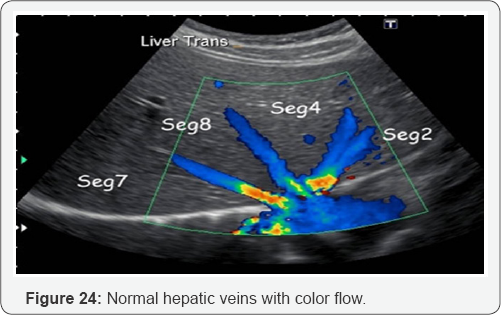
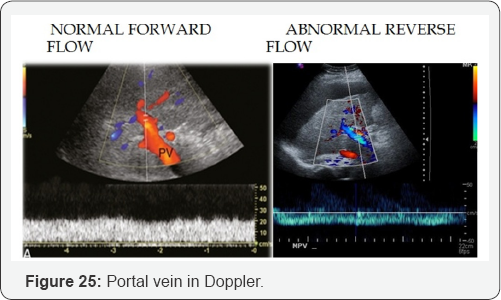
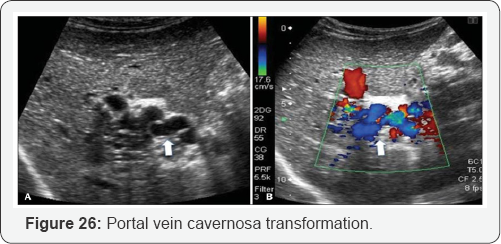
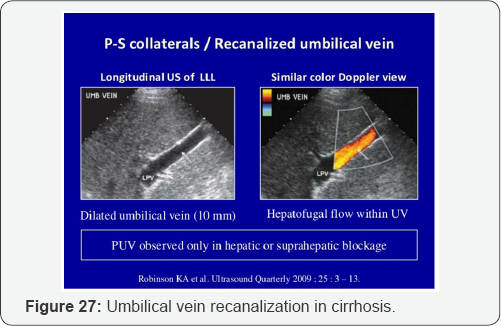
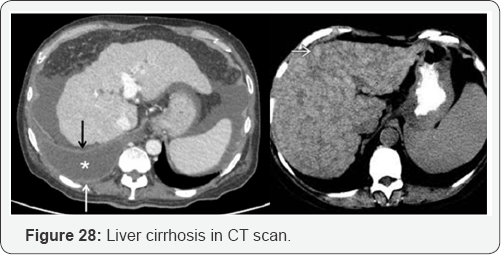
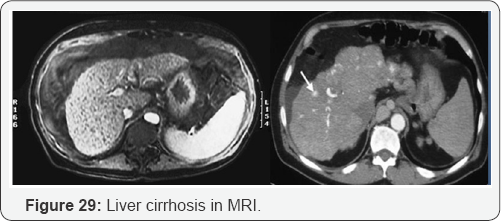
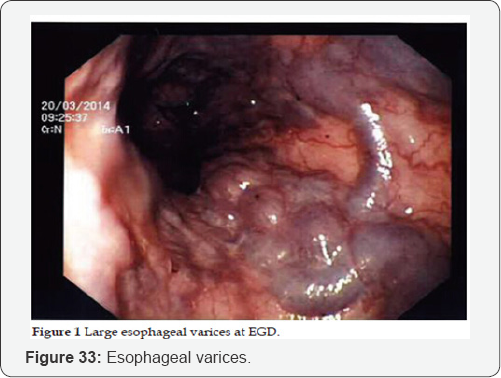
PV dilation due to obstruction. Reverse flow to SMV, IMV, and SV. Blood that cannot enter into PV must return to systematic circulation via anatomotic sites. Results: Esophageal varices, rectal hemorrhoids, caput medusa, etc (Figure 15-29).






Complications
a. Portal hypertension, liver failure and liver cancer
b. Distended abdomen due to ascites.
c. Wasting of muscles.
d. Blood vomiting.
e. Rectal bleeding.
f. Defect in blood clotting.
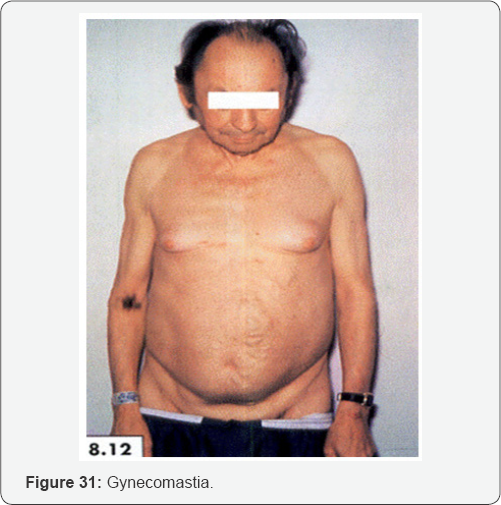
g. Gynecomastia.
h. Spider angioma.
i. Electrolyte imbalance.
j. Caput medusa: Visible veins around the umbilicus.
Results of Liver Failure
a. Accumulation of toxic materials in blood.
b. Decreased production of clotting factors.
c. Decreased production of plasma proteins.
d. Poor metabolism of estrogen.
e. Enzymes abnormalities.
f. Increase Bilirubin.
g. Platelets count decrease.
Conclusion
A. Diagnostic procedures
a. Patient history.
b. Bedside physical exams.
c. Blood works.
d. Ultrasonography of liver (Figure 34).
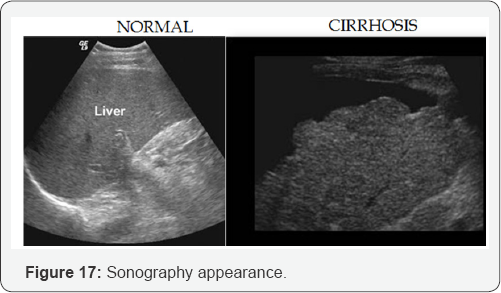
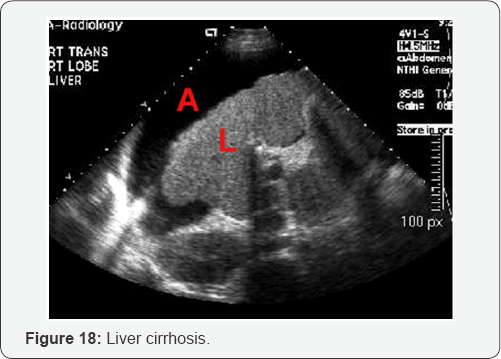
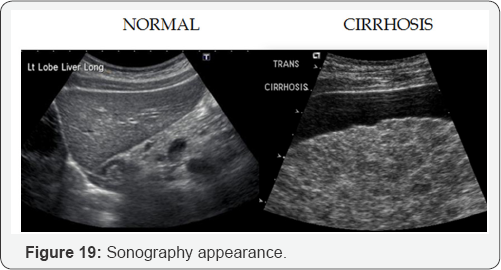
B. Sonographic characteristics of cirrhosis:
a. Hyper echoic liver
b. Course texture.
c. Irregular/nodular surface.
d. Small liver
e. Caudate lobe hypertrophy and decrease echogenicity.
f. Non visualization of hepatic veins.
g. Portal vein dilation >13mm.
h. Portal vein reverses flow.
i. Portal vein hypertension.
j. Dilation of splenic veins, SMV, IMV with reverse flow
k. Splenomegaly.
l. Ascites.
m. Recanalization of umbilical vein [1-11].
For More open access Journals in Juniper Publishers Please click on: https://juniperpublishers.com/
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php




Comments
Post a Comment