Hepatitis B is Increasing in Ethiopian Blood Banks: A Mini Review_Juniper Publishers
ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS
Authored by Hylemariam Mihiretie Mengist
Introduction
The World Health Organization (WHO) estimated that transfusion of unsafe blood accounted for 8 to 16 million hepatitis B virus infections and 2.3 to 4.7 million hepatitis C infections each year [1]. It is estimated that in sub-Saharan Africa, more than 45,000 hepatitis B viruses or hepatitis C virus infections are transmitted through contaminated transfusions annually [2].
Although infectious diseases have many transmission routes, blood donation can be significant avenues for transmission of these diseases to healthy individuals. Most donated blood in Ethiopia is not screened adequately for TTIs due to the lack of a consistent supply of screening reagents and materials. This is a major challenge to the transfusion services in Ethiopia and throughout the underdeveloped world. As a result, use of unscreened blood puts the patient at risk of acquiring many TTIs. Such patients can become potential sources of infection to the community. Consequently, disease burden can impact the entire country and can trigger additional costs for diagnosis and treatment of diseases [3-5].
Prevalence and Associated Factors of Hepatitis B virus
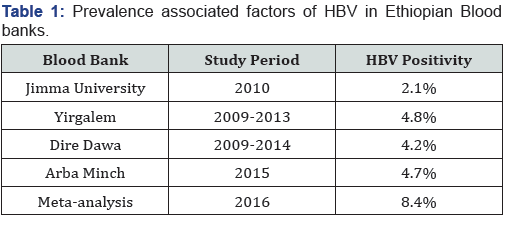
A study reported that the prevalence of HBV in Ethiopian blood banks from 2009-2013 was 4.8% [6]. The prevalence rate of Hepatitis B Virus was 2.1%. Sex and age had statistically significant association with Hepatitis B virus infections where females were less likely to be infected. As age increases above 20 years, the risk of infection with Hepatitis B Virus increases [7].
Prevalence of HBV was 4.7% in Arbaminch Blood Bank. From 17 participants tested positive for HBV, 8 (47%) were males. The test positivity among male was 8/197 (4.1%) while among females was 9/162 (5.6%) and more than three forth participants tested positive were age less than 25. Participants earning 581-1,300 birr were 32.2% less likely to have infection than participants earning below 580 birr per month. Volunteer donors who exposed to unsafe therapeutic drug injection were 11 times increased risk of HBV infection [8]. Among 384 blood donors, 16(4.2%) were positive for HBV in Hawassa Blood Bank [9]. A systematic review and meta-analysis conducted in 2016 showed a pooled HBV prevalence of 8.4% in blood donors [10] (Table 1).
Conclusion
HBV showed increasing prevalence in Ethiopian blood banks. Sex and age significantly affect the prevalence of HBV in? different study areas. Blood banks should use reliable diagnosis techniques to promote safe blood donation.
For more articles in Advanced Research in Gastroenterology & Hepatology please click on https://juniperpublishers.com/argh/index.php




Comments
Post a Comment