Parameters Associated with Risk of Cirrhosis at Diagnosis of Autoimmune Hepatitis in Children_Juniper Publishers
Abstract
Background: Autoimmune hepatitis (AIH) is a
serious chronic and progressive disease. At least a third of patients
have cirrhosis at presentation. Patients with cirrhosis at diagnosis
have a poorer prognosis than those without.
Aim: We aimed to identify parameters associated with risk of cirrhosis at diagnosis of AIH.
Methods: This prospective study included 68
children with AIH. Liver biopsy was performed for all the patients.
Hepatic fibrosis and necroinflammation were evaluated according to Ishak
score. Patients with Ishak fibrosis score 5 and 6 (incomplete and
complete cirrhosis respectively) were compared to the other patients
with Ishak score ≤4.
Results: Children age ranged between 1.5 years
to 16 years. They were 42 females and 26 males. Seventeen (25%) had
cirrhosis. Patients with cirrhosis at presentation had higher mean age
(10.12 years vs. 7.89 years) and were mainly of female sex (82.4% vs.
54.9%). Splenomegaly was more frequent in those with cirrhosis (P
=0.048). They also had lower serum albumin (P = 0.039), longer
prothrombin time (P = 0.04), lower platelets count (P = 0.001) and
higher serum gammaglobulins (P = 0.027). Female sex, splenomegaly, age
≥;9.5 years, albumin ≤3gm/ld,prothrombin time ≥14seconds,platelets
countd200ᵡ103/mm3, and gammaglobulins ≤;2.26 gm/dl were associated with relative risk of cirrhosis ranging between 2.1 and 4.9.
Conclusion: Care should be given to children
with AIH who have parameters associated with relative risk of cirrhosis
at diagnosis as they may need rapid and more aggressive
immunosuppressive therapy to improve the outcome.
Abbreviations: AIH: Autoimmune Hepatitis; ANA: Anti-Nuclear Antibody; AMA: Anti-Mitochondrial Antibody; ASMA: Anti-Smooth Muscle Antibody; ELISA: Enzyme Linked Immunosorbent Assay; NA: Not Available; Type 1 LKM-1: Liver-Kidney Microsomal Antibody Type 1; PT: Prothrombin Time
Introduction
Autoimmune hepatitis (AIH) is a serious chronic and
progressive disease characterized by histological interface hepatitis,
hypergammaglobulinemia, circulating autoantibodies and a favorable
response to immunosuppressive drugs [1,2].
Timely diagnosis and early immunosuppressive therapy is life-saving to
hamper progressive destruction of the liver parenchyma and limit the
development of progressive fibrosis and cirrhosis [3]. AIH has a female predominance. It occurs in children and adults of all ages and affects several ethnic groups [4]. In general, the clinical spectrum of AIH ranges from asymptomatic to severe, with variable symptoms of liver affection [5,6].
The presence of specific antibodies to particular
liver autoantigens is one of the core diagnostic criteria of AIH and its
subtypes. AIH type 1 has been characterized by the presence of
anti-nuclear (ANA) and/or anti-smooth muscle antibodies (ASMA), whereas
liver/kidney microsomal antibodiy type 1 (LKM-1) have been considered as
the hallmark of AIH type 2 [7].
Histologically AIH is characterized by prominent lymphocytic infiltration and varying degrees of lobular hepatitis [8].
At least a third of patients have already cirrhosis at presentation,
indicating that the disease has gone unrecognized for a considerable
period of time prior to diagnosis [9]. Corticosteroid therapy must be instituted early despite the absence of symptoms [10].
The rapidity of improvement rather than the severity of inflammation
may be important in preventing disease progression in mild disease, and
protection can be most reliably obtained by instituting treatment [11].
Patients with cirrhosis and those with bridging necrosis at diagnosis have a poorer prognosis than those without [12,13].
The aim of the current study is to identify parameters associated with
the risk of cirrhosis at the initial liver biopsy at diagnosis of AIH.
Patients and Methods
Study population
This prospective study included 68 children with AIH
recruited from the Pediatric Hepatology, Gastroenterology and Nutrition
department, National Liver Institute, Menofiya University Autoimmune
hepatitis (AIH) group: defined by elevated transaminases,
hypergammaglobulinemia and/or presence of non-specific autoantibodies,
absence of any other etiology and supported by the histopathological
feature of AIH in liver biopsy; according to the international scoring
system [14].
Inclusion criteria were male or female patients with AIH up to the age
of 18 years. Liver biopsy was mandatory for inclusion in the study
Patients with associated liver disease or other immunologic disorders
and those with uncorrected coagulopathy or with contraindication to
liver biopsy were excluded from the study. The study was approved by the
Research Ethics Committee of National Liver Institute, Menofiya
University
Serum autoantibodies and protein electrophoresis
All patients and controls were tested for serum
autoantibodies and gammaglobulins at presentation. ANA, ASMA, LKM-1, and
antimitochondrial antibody (AMA) were tested by indirect
immunofluorescence technique using a Fluoro-KitTM Combo Pak (All from
DiaSorin, Minnesota, U.S.A.). Protein electrophoresis was performed
using Titan III Cellulose Acetate Plate and scanned using Helena
QuickScan 2000.
Serum viral markers, ultrasonography and liver biopsy
Hepatitis B surface antigen (HBsAg), anti-hepatitis B
core IgM and IgG types, were tested for by enzyme linked immunosorbent
assay (ELISA) kit (All from Sorin Biomedica Co, Spain). Hepatitis A
antibody immunoglobulin (Ig)M was tested by ELISA (Diapro diagnostic
bioprobes, Italy). Hepatitis C virus antibody (anti-HCV) was tested by 4th
generation ELISA (Innogenetics, Ghent-Belgium). Real-time polymerase
chain reaction for HCV-RNA was performed using COBAS® Ampliprep/COBAS®
TaqMan®, Roche Molecular Systems, Inc., Branchburg, NJ, 08876 USA.
Ultrasonography (US) was performed by using 2-5-MHz curved linear and
4-8-MHz linear transducers (Xario XG; Toshiba, Tokyo Japan). Liver
biopsy was performed for all the patients using an US guided Tru-cut
needle. Hepatic necroinflammatory activity and liver fibrosis were
evaluated according to Ishak score [15].
Patients with Ishak fibrosis score 5 and 6 (incomplete and complete
cirrhosis respectively) were compared to the other patients with
fibrosis of Ishak fibrosis ≤4.
Statistical analysis
Values were expressed as mean ± standard deviation
(mean±SD) or number (percentage) of individuals with a condition. For
quantitative data, statistical significance was tested by either
independent samples t-test or by the non-parametric MannWhitney U test
according to the nature of the data. For qualitative data, significance
was tested by Chi-square test or Fisher's exact test. Correlation was
tested by Spearman's test. The cutoff values for the significant risk
factors were determined from the receiver- operating characteristic
(ROC) curves. Relative risk was calculated from complex samples
crosstabs statistics. Results were considered significant if P-value
< 0.05. Statistical analysis was performed using SPSS, version 13
(SPSS Inc, Chicago, IL, USA).
Results
Study population characteristics
The current prospective study included 68 children
with AIH. Their ages ranged between 1.5 years to 16 years. They were 42
females and 26 males with female preponderance of a ratio of 2.6.
Fifty-three (77.9%) children were type 1 AIH, only one child (1.5%) was
of type 2 AIH, and 14 children (20.6%) were seronegative for the studied
conventional autoantibodies. All children had liver biopsy performed at
presentation, 17 (25%) of them had cirrhosis.
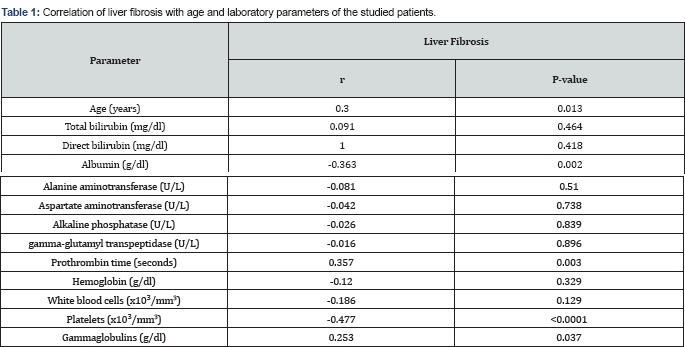
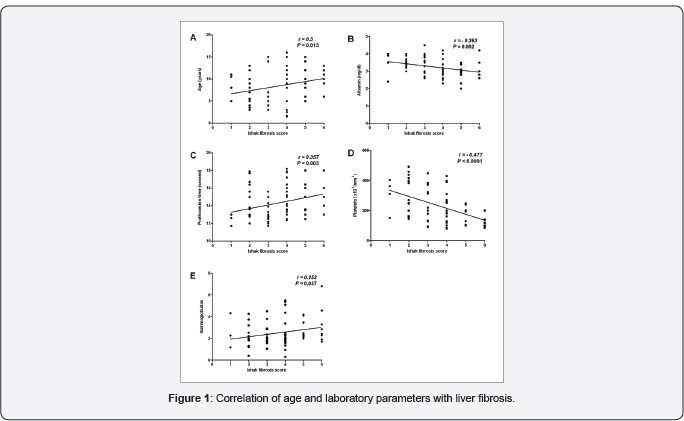
Correlation of the studied parameters with liver fibrosis
All patients, at certain degree, had fibrosis or
cirrhosis at presentation. Age, prothrombin time (PT) and gammaglobulins
correlated directly with fibrosis while serum albumin and platelets
negatively correlated with fibrosis (Table 1 & Figure 1). There was no significant correlation with the other studied laboratory parameters.
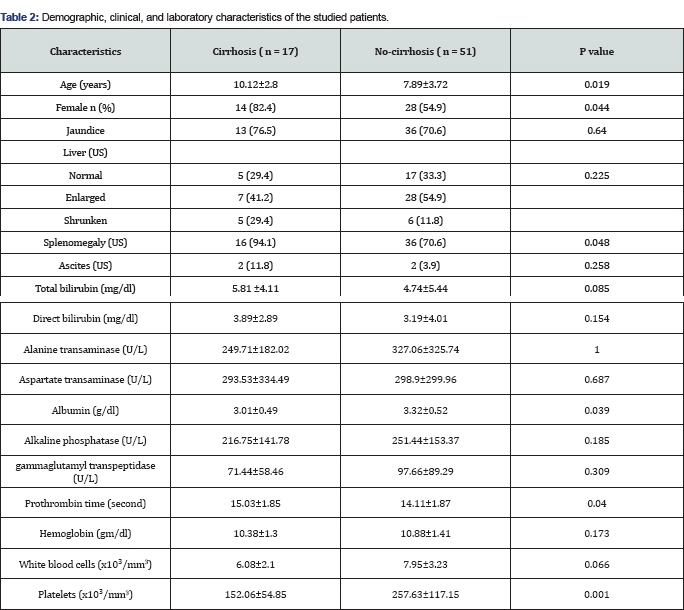
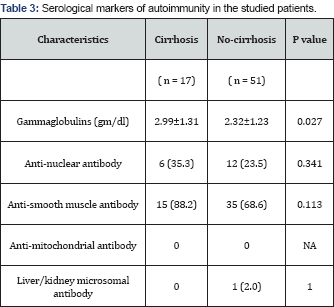
Comparison between children with cirrhosis and those without
Patients who had cirrhosis at presentation in their
initial liver biopsy had higher mean age (10.12 years vs. 7.89 years)
and were mainly of female sex (82.4% vs. 54.9%). Splenomegaly was
significantly more frequent in those with cirrhosis (P =0.048). They had
significantly lower serum albumin (P=0.039), longer PT (P= 0.04), lower
platelets count (P=0.001) and higher serum gammaglobulins (P=0.027)
while other studied parameters were comparable in both groups (Tables 2 & 3).
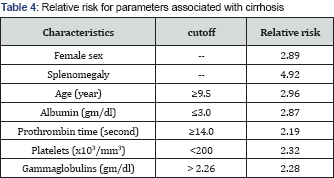
We further determined the relative risk of cirrhosis associated with
parameters with significant difference between the two groups. Female
sex, splenomegaly, age ≥ 9.5 years, albumin ≤3 gm/dl, PT ≥14 seconds,
platelets count ≤200 x103/mm3, and gammaglobulins >2.26 gm/dl were associated with higher risk of cirrhosis ranging between 2.1 and 4.9 (Table 4).
Discussion
Despite the availability of effective treatment, AIH
is not a benign condition. Generally, a high incidence of cirrhosis at
diagnosis in children with AIH has been reported in a number of case
series [16-18]. The current study is concerned with risk factors associated with presence of cirrhosis at the initial diagnosis of AIH.
We found that older age and female sex were
significantly associated with cirrhosis with a relative risk of 2.96 and
2.89 respectively. The higher risk of cirrhosis with older age may be
related to the duration of the disease. This is difficult to ascertain
as the exact start-time of the disease can not be identified and the
disease can start and continue for a considerable time before
manifesting [9].
Another possibility is the adolescence-associated hormonal changes. It
was reported that a flare ofpre-existing disease may occur immediately
before or at the age of puberty especially in females [19]. In accordance with other reports [20,21],
The current study showed a female preponderance with female: male ratio
of 2.6:1. Observations suggest that children and adolescents (age ≤
years) with AIH may have an aggressive phenotype, and may require a more
aggressive management strategy compared to adults (Age > 20 years).
These findings may also reflect differences of immune responses in
different age groups [22].
In the current study, splenomegaly was significantly
higher in those with cirrhosis (94.1% vs. 70.6%) compared to those
without cirrhosis. Those with splenomegaly at presentation have a
relative risk of cirrhosis 4.92 times higher than those without
splenomegaly. This finding is logical as advanced fibrosis and cirrhosis
leads to portal hypertension and its complications. Portal hypertension
usually is diagnosed in children with liver disease when splenomegaly
and/or evidence of portal-systemic collaterals are found during a
physical examination or on abdominal US [23].
According to the laboratory parameters in this study, lower serum albumin (<3g/dl), lower platelet count (<200x103/mm3)
and longer PT (≥;14 seconds) were significantly associated with
cirrhosis with a relative risk of 2.87, 2.32 and 2.19 respectively. In
hand with our findings, Ngu et al. [22] reported that serum albumin <3.6g/ dl (P<0.01), platelet <150x103/mm3
(P<0.01), and international normalized ratio >1.2 (P < 0.01)
were significant predictors for advanced liver fibrosis at diagnosis.
These results suggest that patients with cirrhosis should be offered
prompt treatment to avoid hepatic decompensation [22-25].
Autoantibodies, represent a hallmark in the diagnosis
of AIH, however, neither autoantibody titers at first diagnosis nor
autoantibody behavior in the time course of the disease are prognostic
markers for AIH. Additionally, autoantibody status is unable to predict
immediate outcome after cessation of corticosteroid administration [24,26]. Furthermore, Mehendiratta et al. [2]
reported that the main role of autoantibodies is to identify patients
with AIH and form the basis for a classification, also autoantibody
status did not correlate with disease severity or histopathologic
findings (portal inflammation, piecemeal necrosis, and plasma cell
infiltration). In hand with these reports, we found no significant
difference between patients with and those without cirrhosis regarding
the occurrence of autoantibodies at presentation (P >0.05).
Contrary to autoantibodies, gammaglobulins were
significantly higher in those with cirrhosis (2.99±1.31 vs. 2.32±1.23
gm/ dl; P=0.027) and levels higher than 2.28 gm/dl were associated with
higher risk of cirrhosis (relative risk=2.28). The American Association
for the Study of Liver Diseases [4]
reported that hypergammaglobulinemia >2 times the upper limit of
normal (ULN) indicate a more aggressive disease. The British Society of
Gastroenterology guidelines [27]
suggest that globulins >2 x ULN is considered as evidence of having
moderate to severe inflammation in patients with AIH. Luth et al. [28]
reported that gammaglobulin level is one of the parameters that help in
treatment monitoring in AIH. Furthermore, Puustinen et al. [29] reported that elevated gammaglobulins is a risk factor for cirrhosis of baseline liver biopsy in AIH.
Conclusion
Older age, female sex, splenomegaly, lower serum
albumin concentration ,lower platelets count, higher PT and
gammaglobulins were significantly associated with histopathological
cirrhosis at diagnosis.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment