Eosinophilic Gastroenteritis with Involvement of Duodenum and Colon: A Rare Case with Review of Literature
Authored by Deepankar Kumar Basak
Abstract
Eosinophilic gastroenteritis (EG) is a rare
inflammatory disorder of the gastrointestinal tract of unknown
aetiology. It is characterized by eosinophilic infiltration of the bowel
wall starting from esophagus to rectum most commonly stomach and
duodenum, peripheral eosinophilia and various gastrointestinal
manifestations. Symptoms mainly depend on the affected digestive
segments and the involvement of the different layers of the digestive
wall. Diagnosis requires a high index of suspicion and exclusion of
various disorders that are associated with peripheral eosinophilia. We
report a case of 32 years young man with abdominal pain, vomiting and
loose motion, ultimately diagnose as a case of eosinophilic
gastroenteritis with involvement of duodenum, proximal jejunum and colon
who responded well to steroid.
Introduction
Primary eosinophilic gastrointestinal disease (EGID), originally described by Kaijser [1]
is a rare spectrum of gastrointestinal disorders characterized by
inflammation rich in eosinophils, without evidence of known causes for
eosinophilia, such as parasitic infection, drug reaction, or malignancy [2].
The disease can affect any segments of the gastrointestinal tract from
the esophagus to the rectum, giving rise to various clinical
presentations including Eosinophilic Esophagitis (EE), eosinophilic
gastritis, eosinophilic gastroenteritis(EG) and Eosinophilic Colitis
(EC).
Eosinophilic esophagitis and gastroenteritis is more
common but EC is exceptionally rare with only a few cases being reported
since 1979. The absence of defined histological criteria for a specific
eosinophils count in the colonic mucosa makes the diagnosis of this
entity challenging. Hence, its true frequency is not clear. The clinical
presentation includes abdominal pain, diARGHhea (bloody or non-bloody),
and/or weight loss. EC in its primary form can be associated with other
atopic conditions. Colonic eosinophilia cans also occured secondary to
helminthic infections (e.g. pinworms, hookworms), inflammatory bowel
disease, autoimmune disease (e.g. scleroderma, Churg Strauss syndrome),
celiac disease, drug reactions and in association with the HES.
Since secondary eosinophilic inflammation may occur
in numerous gastrointestinal disorders such as IgE-mediated food
allergy, gastro esophageal reflux disease and inflammatory bowel
disease, the true incidence and prevalence of primary EGID remains
largely unknown. A recently established world- wide-web registry found
that EGID mainly affects the pediatric population, although it has been
reported in patients up to 68 years of age [3].
In the past few years, EE has been increasingly recognized as a
distinct condition that affects about 1% of the population, and accounts
for dysphagia and food impaction that remain nonresponsive to
traditional anti-reflux management, both in pediatric and adult
gastroenterology [4]. Accordingly several excellent reviews on EE have recently been published [4-6].
In contrast, EC represents the least frequent manifestation of EGID
whether or not it presents with disease in other segments of the
gastrointestinal tract. 3 EC appears to have a bimodal distribution that
affects neonates with a relatively high prevalence and a separate group
of young adults with no gender preference.
Case Report
A 32-years-old young man was admitted with 1 week
history of progressive abdominal discomfort, vomiting and diARGHhea
which was aggravated by taking meals. Stool was watery in nature,
10-12times/day but not mixed with blood. He mentioned similar type
symptoms many times but last one was few months back, since then he lost
4 kg wt. He had no history of abdominal surgery or any known food
allergy. He had a history of skin disease from childhood, most probably
ichthyosis vulgaris, for this reason he currently not taking any
treatment. He denied taking any drugs or herbal medicines. On clinical
examination, he appeared dehydrated and vitals were normal. His abdomen
was soft and slightly distended. Laboratory investigations showed a high
white cell count of 16.3x109/L, with raised eosinophils count of
40.1x109/L. The hemoglobin level and platelet counts were normal. The
liver function tests, erythrocyte sedimentation rate, C-reactive protein
and autoimmune antibody screen were normal. The serum immunoglobulin-E
(IgE) was highly raised at 1044IU/ml (normal reference range, less than
128IU/ml). Stool culture for pathogens and analyses for ova, cysts and
parasites were negative. USG of abdomen and x-ray abdomen was
unremarkable. Skin consultation was taken and diagnosed as ichthyosis
vulgaris for this reason treatment is started.
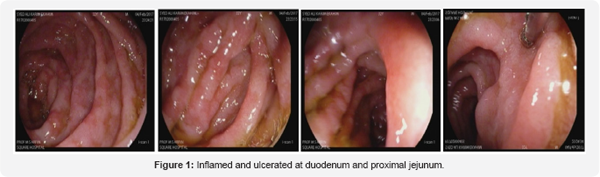
Endoscopy revealed mild form of monilial esophagitis
at lower end of esophagus but mucosa of at the bulb and post bulbular
area, second part of duodenum and proximal jejunum is severely inflamed
and ulcerated at places (Figure 1). Multiple Biopsies was taken from duodenum and proximal jejunum.
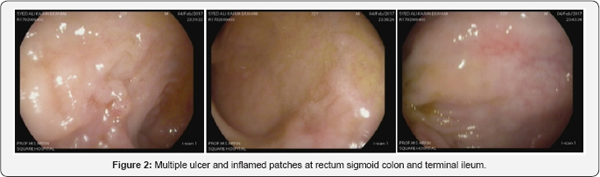
On colonoscopy showed multiple ulcers and inflamed
patches at the rectum and sigmoid colon. Multiple ulcers and heaped up
lesions is seen at the terminal ileum (Figure 2). Biopsy was taken from terminal ileum and rectum.
Biopsy report of duodenum and proximal jejunum
revealed diffuse infiltration of inflammatory cells including a fair
number of eosinophils (>40/hpf). Small number of plasma cells,
lymphocytes & polymorphs are also present. The surface is focally
eroded. No evidence of malignancy is seen.
Biopsy report of rectum and sigmoid colon showed
focal erosion. Lamina propia shows mild congestion and diffuse
infiltration of a fair number of eosinophils and plasma cells.
Eosinophilic cystitis is noted lymphoid follicle is formed.
Mucosa of terminal ileum showed some of villi are
shortened and broad. The lamina propia shows dense infiltration of
chronic inflammatory cells including fair number of eosinophilic and
plasma cells. Lymphoid follicles wit prominent germinal centre are
present. Surface is focally eroded.
He was treated with oral prednisolone (30mg daily).
His symptoms improved and the serum white cell and eosinophils counts
returned to normal levels after 5 days. The steroid dose was gradually
tapered at follow-up as outpatient and successfully stopped a year
later. He has remained symptom-free for more than 3 years
post-treatment.
Discussion
Eosinophilic gastroenteritis is a rare, benign
inflammatory disorder of the gastrointestinal tract, characterized by
Eosinophilic infiltration of the bowel wall, in the absence of known
causes of Eosinophilic, including drug reaction, parasitic infections
and malignancy [1,3].
Eosinophils in the gastrointestinal tract are responsible for innate
immunity to parasites, regulation of lymphocytes, antigen presentation
and protection against tumors. Nevertheless, over-stimulation of
eosinophils generates excessive degranulation which can lead to severe
inflammation, production of neurotoxins and reactive oxygen species
which are responsible for the typical symptoms of eosinophilic
gastroenteropathy [6,7].
EGID in general has three hallmarks including
peripheral eosinophilia (typically in the range of 5% to 35%), segmental
eosinophilic infiltration of the gastrointestinal tract and functional
abnormalities [7,8].
Importantly, up to 23% of patients with primary EGID have no peripheral
eosinophilia. EG affects all ages of both genders and diagnosed most
frequently in the third decade of life [2,3]. EG mainly involves the stomach and duodenum [1,2].
The pathogenesis and aetiology remain unclear A personal or family
history of allergic disorder is reported in 70% of patients with this
disorder.
EG should be considered in the differential diagnosis
of unexplained gastrointestinal symptoms, especially in the presence of
peripheral eosinophilia. The 3 main diagnostic criteria are:
- The presence of gastrointestinal symptoms.
- Biopsies showing eosinophilic infiltration of one or more areas of the gastrointestinal tract (>20 eosinophils per high power field) or typical radiological findings with peripheral eosinophilia.
- No evidence of parasitic or extra-intestinal disease. Histopathology is the gold standard for diagnosis [1,3]. Depending on the location of the compromised tissue, eosinophilic gastroenteropathy may be identified as esophagitis, gastritis, duodenitis or colitis. The last is exceptionally rare and only a few cases have been reported since 1979. It has very non-specific symptoms of fever, diARGHhea, abdominal pain and weight loss.
In 1970, Klein classified this disease according to the depth of involvement:
- The Mucosal Form (25% to 100%) most often affects the stomach and is manifested by anemia, fecal blood loss and weight loss.
- The Muscular Form (13% to 70%) manifests through nausea, vomiting, diARGHhea, abdominal cramps, and intestinal obstruction.
- The Serosal Form (12% to 40%) manifests through eosinophilic ascites, high levels of peripheral eosinophilia and severe inflammation [8,9].
EG is usually patchy in distribution. Invasive
laparotomy or laparoscopic full thickness biopsy may need to be
performed to diagnose subserosal disease. Peripheral eosinophilia is
seen in up to 80% of cases of EG [2,3].
Raised serum IgE, as seen in our patient, was reported to be more
prevalent in children with EG. A multidisciplinary task force has
recently reached consensus on the diagnostic criteria of EE, including
the presence of more than 15 eosinophils per high-power field in the
esophageal squamous mucosa. No such consensus exists for EG & EC,
although most authors have used a diagnostic threshold of 20 eosinophils
per high-power field. Of note, normal values for tissue eosinophils
vary widely between different segments of the colon, ranging from 30 in
the caecum, thus location of the biopsy is critically important for
interpretation of findings.
More or less prominent tissue eosinophilia in the
colon may result from a number of conditions and EC remains therefore a
diagnosis of exclusion. Colonoscopic biopsies obtained from patients
with inflammatory bowel disease, in particular with Crohn's colitis,
often show severe tissue eosinophilia. Parasitic infection of the colon
with pinworms, roundworms, or whipworms may lead to marked eosinophilic
infiltration, and repeated stool or serological testing may be needed to
reveal this specific etiology. Drug-induced EC has been described in
response to clozapine, carbamazepine, rifampicin, non-steroidal
anti-inflammatory agents, tacrolimus and gold. EC has also been
associated with autoimmune connective tissue disease including
scleroderma, dermatomyositis and polymyositis as well as with allogeneic
bone mARGHow transplantation and the rare Tolosa- Hunt syndrome that
features inflammatory ophthalmoparesis. The idiopathic hypereosinophilic
syndrome (HES) may also affect the colon, but this rare condition
presents with sustained and marked peripheral eosinophilia with
end-organ damage that extends beyond the gastrointestinal tract (e.g.
heart and skin).
Diagnosis of 80% of these patients is done through
upper digestive tract endoscopy of the stomach and small intestine and
colonoscopy with tissue biopsy. In most cases, macroscopic study of the
gastrointestinal mucosa shows normal mucosa, slight edema and
congestion, and even ulcers or lesions with nodular configurations.
Ninety percent of patients with EG respond to steroid therapy, and more
dramatic response is usually seen in the serosal subtype [2,3].
The duration of steroid therapy reported in the literature is variable.
Other treatment options include dietary modification, leukotriene
receptor antagonists, mast cell stabilizers, and antibodies against
interleukin-5 and IgE [1,3,5].
Surgical intervention may be required for cases where a definitive
diagnosis cannot be made or when perforation or significant obstruction
occurs [1,3].
The natural history of EG is unclear, emphasizing the need for
long-term follow-up studies for patients with EG. Our patient needs to
follow-up [10,11].
Conclusion
In summary, we present a rare case report of
Eosinophilic gastroenteritis and colitis diagnosed on histopathology and
respond to steroid therapy. Clinician should be aware of this rare
entity as it can mimic several other gastrointestinal disorders.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment