Constipation and Biofeedback; Important Gastrointestinal Symptom but Ignored Initial Management
Authored by Ozdal Ersoy
Abstract
Constipation is the most common digestive complaint
in the general population and its etiology is diverse. Defecatory
disorder is a common type of constipation where the patient has
difficulty during evacuation due to ineffective relaxation of the anal
sphincter and/or inadequate abdominal push. Biofeedback therapy for
constipation is a technique used to train a patient's mind to control
the way their anorectum works. Biofeedback therapy is unfortunately not
available in many centers and also not widely recommended by the
physicians although its response rate in the treatment of constipation
is about 70-80%. Here, the constipation and biofeedback therapy are
shortly reviewed under the light of recent literature and, our study
observing the percentage of patients who performed BFT in real world
upon recommendation and its clinical response rate in our center for
anorectal disease as well as the bARGHiers to biofeedback is discussed.
Keywords: Constipation, Biofeedback, Dyssynergy, Defecatory, Anorectal manometry, Balloon expulsion test
Abbreviations: BFT: Biofeedback Therapy; UK: United Kingdom; ARM: Anorectal Manometry; BAT : Baloon Expulsion Test
Introduction
In order to defecate properly, one needs to be full
first and also has to know that he/she Is full, then he/she also has to
go to squeeze well (able to hold the stool) until sitting on a toilet.
When reached to the toilet, the last but the other two important steps
are to open (relax) the back-passage to open the bowel and then close it
back when he/she feels completely empty. If any of these steps is
deranged by somehow, functional constipation can occur.
Constipation is the most common gastrointestinal
disorder in adults and may be regarded as disordered movement of stool
through the colon or anorectum since, with few exceptions, transit
through the proximal gastrointestinal tract is often normal. Slowing of
colonic transit may be idiopathic or may be due to secondary causes.
Constipation is simply defined as bowel symptoms (difficult or
infrequent passage of stool, having hard stool and excessive straining,
feeling of incomplete evacuation, need for digital maneuvers) that may
occur either in isolation (primary) or secondary to another underlying
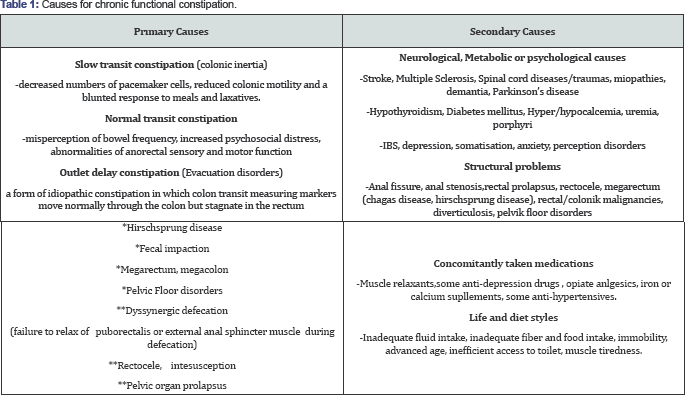
disorder Etiology of constipation is summarised in Table 1 and extensive list of other causal factors is well described elsewhere in the literature [1].
It is also very important to remember that, constipation can be drived
from a singluar entity or multiple overlapping etiologies which may lead
to the need for basic or advanced treatment modalities.
Very careful and meticulous history taking (duration
of the symptom, consistency of the stool, defecation frequency and the
need of digital maneuvers and excessive straining, sensation of
incomplete evacuation, concomitant drug use and diseases, alarm
symptoms) and physical examination (especially rectal digital
examination including squeeze and pushing maneuvers) are valuble
elements for the initial assessment of the patient with chronic
constipation. Laboratory evaluation, endoscopic evaluation, radiology
studies and anorectal physiology testing (ARM, anorectum sensations,
BAT) should be performed only in selected individuals. Anorectal
manometry with or without BAT, is a valuable diagnostic test especially
in patients with evacuation pathologies [2].
As an initial management of constipation,
conservatory treatment (patient education, toileting habits and behavior
modification, trial of dietary changes, trial of fiber, basic laxative
therapy and bowel retraining and/or biofeedback) without diagnostic
testing can be considered when alarm features are absent. Severe,
intractable, slow transit constipation is rare and may be treated with
surgery, but with extreme caution; patients should be referred to
specialized centers for a full evaluation prior to surgery if needed [3].
Dyssynergic defecation which is a grossly
unrecognized evacuation problem and a particular type of chronic
constipation, means a dyscoordination between the rectum and the anal
sphincter and puborectalis muscles during defecation. In patients with
dyssynergic defecation, defecation is ineffective due to failure of the
anal sphincter to relax, or inappropriate contraction of the
puborectalis and external anal sphincter muscles or inadequate abdominal
propulsive force to increase theintrarectal pressure (pushing failure) [4].
These patients usually have life-long constipation and experience
significant difficulty with passing stools but are unaware that they
have this type of constipation. However, they often don't seek help
beyond using over-the-counter laxatives, and some doctors also aren't
aware of the condition either, therefore and consequently these patients
cannot be treated well.
However, BFT is not widely available and used; it has
not been well standardized among the trainers therefore the results may
vary at different centers. However, where available, it is simple,
attractive, alternative and satisfactory for patients especially with
pelvic floor dysfunction (dyssynergic defecation) and severe
constipation as it retrains the pelvic muscles and provides the
potential for treatment without laxatives and protects the patients from
over performed or complicated colorectal surgeries (e.g.
hemorrhoidectomy, sphincterotomy, colonic resections).
In the literature, many methods of BFT can be
observed. Various instruments, including anal plugs rectal balloons, and
anorectal manometer catheters, have been used to monitor external anal
sphincter pressures during attempted expulsion of the apparatus. The
patient watches/ hears the recordings of sphincter pressure traces or
EMG activity and is asked to modify inappropriate responses through
trial and error, this type of BFT is known as visual/auditory BFT.
During visual biofeedback training, a probe with sensors is inserted
rectally which the sensor detects the muscle signals from the anus and
rectum and displays them visually
on a TV monitor. While sitting on the commode the subjects are able to
see how these muscles are contracting or relaxing and with the visual
feedback learn how to coordinate them correctly to improve their push
and relaxation movements. Generally the patient attends to this type of
sessions once a week for 4-6 weeks therapy Unfortunately it is only
offered at few specialized centers because insurance generally do not
cover this rarely recognized treatment modality [7].
Whereas UK type bowel retraining/biofeedback programmable assessment
ofthe patient' s bowel symptoms, general health, diet, any medications
and other psychosocial factors that may influence the patient's bowel
function. Using this information and the results of any investigations
that the patient may have had, the nurse discusses the likely causes of
the problems and plans a treatment programme for the patient to work on
together. The therapy involves teaching the patient how to retrain the
muscles used to empty and control the bowels and the nurse shows the
patient (lying on left lateral position) how to use his/her muscles
while the patient is simulating defecation with a balloon inside his/her
ano rectum during a minimum one hour lasting session. Most patients
have one or two further appointments or phone call- interviews (with the
same physician/nurse) at approximately one or two month intervals [8].
All biofeedback techniques aim people to be more aware of unconscious
or involuntary bodily functions involved in defecation and help
individuals relearn the normal process of having a bowel movement
As mentioned before, BFT is not universally available
in many centers where constipated patients are seen. Like in Turkey,
clinical trials about the efficacy of biofeedback in anorectal disorders
and pelvic floor dysfuntions are very rare because of lack of centers
and/or medical stuff (physician, pelvic floor physiotherapist and/ or
continence nurse) performing or recommending BFT to the concerned
patient.
In our study, we retrospectively observed 437
patients who were referred to our 'Center for anorectal diseases'
between 20132016 .We did the study to find out primarily: what
percentage of the patients with constipation who are recommended BFT had
performed BFT in real-life and what are the main obstacles for not
attending to BFT. Secondary aim was to find the success rate and its
factors of BFT.
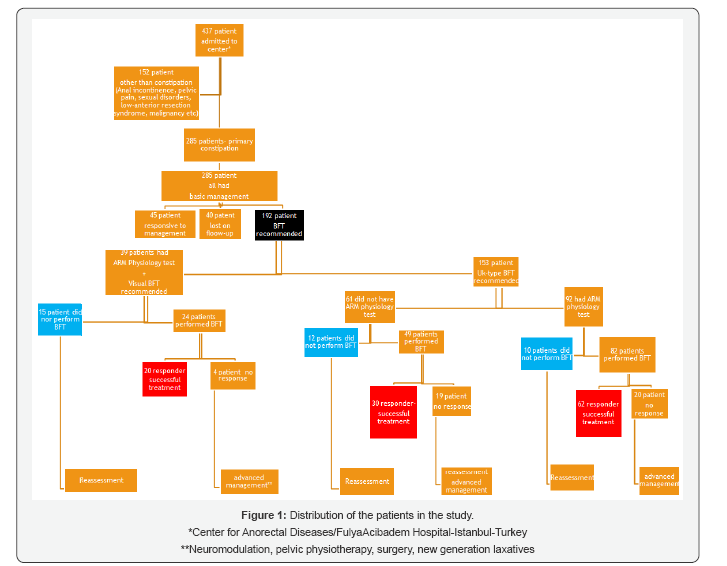
The study showed that, among 437 patients, 285 had
chronic functional constipation and/or its complications (haemorrhoids,
anal fissure). After the initial assessment of the constipated patients,
all are recommended basic/standard managements (patient education,
correct toilet positioning, planning convenient toileting habits, and
behavior modification, trial of dietary changes, trial of fiber, basic
laxative therapy) and then the patients are called back to control
visits after 4-6 weeks. Fourteen percent of the patients are lost during
follow-up and 16% of them had corrected bowel function at the end of
4-6 weeks of standard therapy. The rest, 192 patients who were
unresponsive basic managements, had performed bowel retraining (UK-type
BFT or visual BFT). Both types of BFT are performed under the guidance
of both physician and physiotherapist/nurse. Visual BFT is performed in
patients only after anorectal physiology tests (anorectal manometry,
anal/ rectal electrical sensation test, balloon expulsion test and/or
defecography) had been performed; whereas for 40 % patients whom UK-type
BFT was performed had no anorectal physiology tests done previously.60%
of the patients who were referred to visual BFT, did attend to their
BFT sessions and bowel movement improvement was possible in nearly 85%
of patients through biofeedback whereas 90% of patients who were
recommended UK-type BFT after physiology tests performed, did attend to
their BFT and 75% of these patients showed improvement in their
symptoms. Among patients whom UK-type BFT is performed without
performing any anorectal physiology tests, 80% of them performed BFT
with the success rate of 60%. The patients who did not perform BFT, are
followed up and reassessed for the reasons and the patients who did not
get any improvement with BFT, advanced treatment modalities and/or
further diagnostic tests are discussed and/or planned. Summary of the
patients (in numbers) are summarised in Figure 1
The main reasons for not performing visual BFT when
recommended are; being expensive (due to different coverage problems by
health insurance companies), being not common in Turkey thus showing
doubt to treatment, long duration of treatment (once a week for at least
6-8 weeks) and transportation problems due to living in long distance
from the center. Whereas the main reason for not to apply UK-type BFT is
the doubt to treatment modality probably due to the heterogenity of the
description of BFT. The cost and the treatment durations seem to be
negative factors for visual BFT in our study. When BFT (both kinds) is
recommended after physiology tests are done, number of patients who
accepts to perform BFT is more than the ones who did not perform the
anorectal tests before. The BFT is more effective in patients with
defecatory symptoms rather than slow transit constipation and also more
success is observed in highly motivated and interactive patients during
the sessions.
Discussion
Chronic constipation is a well known and a frequently
seen symptom in many medical clinics but unfortunately less attention
is given to the appropriate non pharmacological treatment modalities
like BFT. It is a chronic debilitating problem for the patient with
significant negative impacts in quality of life and social functioning
however many patients still do not have much knowledge about BFT
modality due to the less availability
Functional constipation (without any organic cause)
is a learned behavior, so it can be unlearned as well via BFT. It aims
to bring about symptom relief by teaching good evacuation dynamics, to
improve sphincter coordination and tone, and replace bad toileting
behavior with normal habits and to decrease stress/worry by explaining
symptoms and encouraging realistic expectations. During BFT trained
therapists-including physicians, nurses, and physical or occupational
therapists-teach patients strengthening exercises or relaxation
techniques that can be performed to reduce their symptoms. The sessions
vary in number, length and frequency, and techniques can take place in a
doctor's office and be continued at the patient's home. Biofeedback, in
constipated patients is associated with improved gut transit and
autonomic innervation [9].
Randomized controlled trials from specialized centers
report response rates of 60%-80% for defecatory disorders. Whether this
therapy is as successful outside of trials or specialized centers
remains unclear.BFT is an effective outpatient treatment for
constipation in long term as well as it is non-invasive, free from side-
effects and well tolerated. However, real life experiences about BFT
shows that less than half of patients recommended BFT undergo the
therapy [10].
As also observed in our study, the main causes of this, is the
difficulty in its availability, the paucity of the specialized centers
and the trainers and insurance-coverage policies. If these obstacles are
overcome, the success rates in many hetero genous populations
undergoing BFT are only slightly less than published randomized trials
as it is also seen in our study
Conclusion
Constipation is one of the most common digestive
problem and Nearly 25-30% of affected people have dyssynergic
defecation, in which muscles used for bowel movements do not work well,
however BFT is labor-intensive and very effective when well- done for
defecatory disorders but unfortunately BFT use is not as common as it is
needed. Thus, both the physicians and the patients need to be trained
and motivated about the use of BFT more widely and prospective trials or
real-life experiences are war rented to handle the bARGHiers to BFT.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment