Effective Optical Identification of Depressed Type �0-IIc� Early Primary Nonampullary Duodenal Neoplasms with NARGHow Band Imaging Magnification Endoscopy
Authored by Nikolas Eleftheriadis
Abstract
Aim: The efficacy of NARGHow-Band Imaging
Magnification Endoscopy (NBI-ME) in evaluation of early primary
NonAmpullary Duodenal Neoplasm (NADN) is studied.
Material and Methods: Three patients with
depressed type '0-IIc' early NADN, two duodenal adenomas (a 32-years-old
male with familial adenomatous polyposis and a 60-years-old male with
dyspepsia came for screening gastroscopy) and one case with NADN
adenocarcinoma, endoscopically identified by NBI-ME upon indication, is
reported. White light endoscopy showed a superficial redness.
Indigo-carmine chromoendoscopy showed better visualization of the
lesions.
Results: In the early NADN carcinoma, NBI-ME
with maximum (X80) magnification, clearly revealed specific abnormal
mucosal microsurface and microvascular findings, particularly an
irregular inter-lobular loop (ILL-1) pattern, while NBI-ME after acetic
acid spray showed higher endoscopic images of tumorous mucosal pattern
microstructures (fusion and increased intensity of villous structures),
according to previous classification for early gastric cancer.
Demarcation line was also clearly identified. Successful curable R0
endoscopic resection followed, two endoscopic mucosal resections (EMRs)
and one endoscopic submucosal dissection (ESD). ESD resection was based
on NBI-ME findings. Histology showed two duodenal adenomas and one
mucosal duodenal adenocarcinoma.
Conclusions: NBI-ME in combination with acetic
acid spray is a useful method for optical characterization of early
NADN. Further studies are necessary.
Introduction
Early, primary non-ampullary duodenal (adenoma or
adenocarcinoma) (NADN) is an extremely rare disease that is confined to
mucosa or submucosa and does not touch the papilla of Vater. Under
conventional white light endoscopy (WLE) in combination to
indigo-carmine chromoendoscopy NADNs may appear as flat or slightly
depressed lesions resembling more than gastric lesions [1,2].
NARGHow-band imaging magnification endoscopy (NBI-ME)
has been effectively used for real time, optical diagnosis of
superficial gastric and colorectal lesions [3-12], with specific standardized classifications [10,13]
are routinely in use by Japanese experts; however international
experience for duodenal lesions is limited, while no standardized NBI-ME
classification has been yet reported for such rare lesions.
Endoscopic resection, either endoscopic mucosal
resection (EMR) or endoscopic submucosal dissection (ESD) are the
treatment of choice for early duodenal neoplasms as well, however these
procedures in duodenum are more challenging and demanding, with higher
risk of complications, such as perforation or bleeding, even in experts
hands [1].
Preoperative evaluation is important to identify
lesions in early curable stage, which can be treated by endoscopic
resection. Furthermore, endoscopic histology in real-time by NBI-ME
could provide a higher diagnostic value for surveillance of
periampullary and nonampullary adenomas in FAP patients, according to
rare reports [1,2].
The aim of the present study is to report on three
cases of depressed type '0-IIc' early NADN, two cases with duodenal
adenomas and one case with primary early adenocarcinoma, successfully
identified endoscopically, by NBI-ME upon indication.
Material and Methods
We report on three patients with depressed type '0-IIc' (JCGC [14] & Paris endoscopic classification[15])
early NADNs, two patients (a 32-years-old male with FAP and a
60-years-old male with dyspepsia came for diagnostic upper
gastrointestinal (GI) endoscopy), with duodenal adenomas and one case
with primary early nonampullary duodenal adenocarcinoma, successfully
identified endoscopically, by NBI-ME upon indication. Personal and
family history was negative. They reported no smoking, alcohol, medicine
or other drug use.
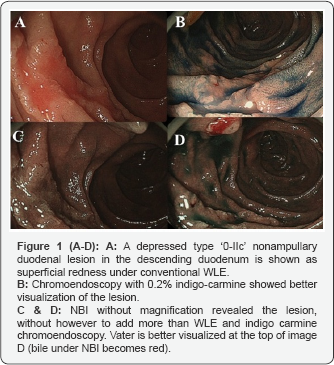
Under conventional WLE all lesions showed a depressed type superficial redness (Figures 1A, 3B & 4A).
Indigo-carmine chromoendoscopy resulted in better delineation of the
type '0-IIc' duodenal lesions, but no further abnormalities (Figures 1B, 3D & 4B). NBI without magnification (Figures 1C-1D & 3D) showed better the duodenal lesions and the papilla of Vater (bile under NBI became red colored, Figure 1D), however without any advantage to WLE or indigo carmine chromoendoscopy, regarding the endoscopic tissue characterization.
Patient with primary early NADN adenocarcinoma (Showa University)
In the case of nonampullary duodenal adenocarcinoma,
endoscopy was performed in the Digestive Disease Center of Showa
University, Japan. Before endoscopic evaluation, a solution of pronase
20000 units (Pronase MS; Kaken Pharmaceutical Co, Ltd, Tokyo, Japan) and
sodium bicarbonate 1gr diluted with 0.2% simethicone 80ml (Gascon;
Kissei Pharmaceutical Co, Ltd, Nagano, Japan) was administered in order
to remove mucus. A high resolution, zoom video-endoscope with NBI
(H260Z; Olympus Medical Systems, Co, Ltd, Tokyo, Japan) and an electric
endoscopic system (EVIS 260 LUCERA SPECTRUM; Olympus Medical Systems)
was used for this examination. A hood (D- 201-12402 Olympus) was mounted
on the tip of the endoscope to enable the endoscopist to fix the focal
distance between the tip of the endoscope and the gastric mucosa at
approximately 2mm for NBI imaging. The hood was also useful in
identifying the duodenal lesion and marking the borders of the lesion
before endoscopic ESD resection. Under moderate sedation with diazepam
and fentanyl, as needed, O2 and monitoring, diagnostic upper digestive endoscopy was performed, at endoscopy department of the Digestive Disease Center.
Patient with FAP came for routine, yearly diagnostic UGI endoscopy
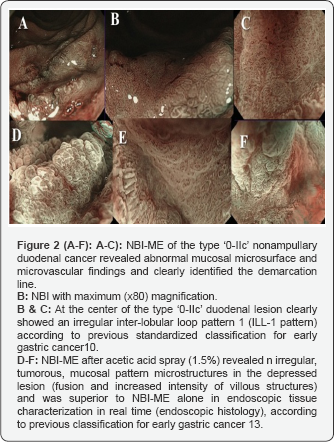
A 30-years-old male with familial adenomatosis
polyposis (FAP) who underwent total colectomy with ileal anal pouch
anastomosis, came for routine yearly diagnostic upper GI endoscopy.
Known multiple fundic gland gastric polyps were found (Figure 3A), while, unexpectedly a small (0.5cm) depressed type '0-IIc' NADN was also identified (Figure 3B), which was not found a year earlier.
Patient with dyspepsia came for follow-up endoscopy
A 60-years-old male came for follow-up diagnostic
gastroscopy due to dyspeptic symptoms. He reported a previous history of
coronary heart disease and was under anticoagulants. A small (0.5cm)
depressed type '0-IIc' NADN was again unexpectedly found under WLE (Figure 4A), which was not found a year earlier.
Results
Patient with primary early NADN adenocarcinoma (Showa University)
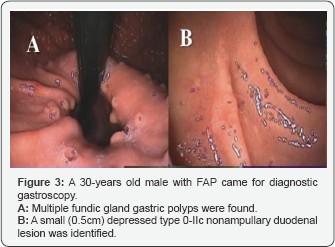
In the particular case of a patient with nonampullary
duodenal carcinoma, NBI-ME with the maximum magnification (X80) at the
center of the lesion (Figure 2A-2F),
enabled the observation of specific abnormal mucosal microsurface and
microvascular findings, particularly an irregular inter-lobular loop
pattern 1 (ILL-1)10 (Figures 2A-2C), according to previous standardized classification for early gastric cancer10. Demarcation line was also clearly identified (Figure 2B).
Furthermore, NBI-ME after acetic acid spray showed
clear irregular (tumorous) mucosal pattern microstructures with fusion
and increased intensity of villous structures (Figures 2D-2F)
and was superior to NBI-ME alone in endoscopic tissue characterization
in real time, according to previous classification for early gastric
cancer [13].Furthermore,
NBI-ME after acetic acid spray showed clear irregular (tumorous)
mucosal pattern microstructures with fusion and increased intensity of
villous structures (Figures 2D-2F)
and was superior to NBI-ME alone in endoscopic tissue characterization
in real time, according to previous classification for early gastric
cancer [13].Furthermore,
NBI-ME after acetic acid spray showed clear irregular (tumorous)
mucosal pattern microstructures with fusion and increased intensity of
villous structures (Figures 2D-2F)
and was superior to NBI-ME alone in endoscopic tissue characterization
in real time, according to previous classification for early gastric
cancer [13].Furthermore,
NBI-ME after acetic acid spray showed clear irregular (tumorous)
mucosal pattern microstructures with fusion and increased intensity of
villous structures (Figures 2D-2F)
and was superior to NBI-ME alone in endoscopic tissue characterization
in real time, according to previous classification for early gastric
cancer [13].
Based on the above-mentioned NBI-ME findings
endoscopic prediction of histology and differentiation type was made
with high accuracy. The NBI-ME findings were suitable to well-
differentiated duodenal adenocarcinoma confided to the mucosa, which was
also subsequently proved by full histopathologic examination of the ESD
specimen. Based on the NBI-ME findings precise tumor margin marking and
successful curable R0 endoscopic ESD resection followed. Histopathology
of ESD specimen showed early mucosal duodenal adenocarcinoma.
Patient with FAP came for routine, yearly diagnostic UGI endoscopy
In the male with FAP, indigo carmine chromoendoscopy
visualized better the duodenal lesion, particularly the borders of the
lesion (Figure 3C), while NBI without magnification did not add more to WLE or indigo carmine chromoendoscopy (Figure 3D). Histological examination of biopsy specimens showed duodenal adenoma (type III according to Vienna classification [16]).
Endoscopic en bloc R0 resection was followed by EMR-C and three clips
were placed to close the EMR ulcer, in order to prevent late
complications, such as perforation or bleeding (Figure 3E). H&E stain of the EMR specimen showed duodenal adenoma (type III Vienna classification [16]), with complete pathological rejection (Figure 3G).
.png)
Patient with dyspepsia came for follow-up endoscopy
In the patient with dyspepsia, indigo carmine chromoendoscopy visualized better the lesion (Figure 4B).
Histology of biopsy specimen showed adenoma and endoscopic resection
was followed after stopping anticoagulants. Finally endoscopic en bloc
R0 resection by EMR-C was completed (Figures 4C &4D) and three clips (Figure E)
were placed to close the EMR ulcer (fig. D), in order to prevent late
complications, such as perforation or bleeding. Histology showed
duodenal adenoma (type III Vienna classification [16]) with complete pathological resection. One year later a normal scar was identified and no residual tumor (Figure 4F).
.png)
Discussion
Early endoscopic detection with subsequent complete
endoscopic resection is the best strategy for optional outcome of GI
cancer, including duodenal neoplasms [3,17,18].
Early primary nonampullary duodenal adenocarcinoma however, is an
extremely rare disease, may appear as small flat area, usually depressed
type '0-IIc' lesion (Paris classification [15]),
as in our cases, which resembles more to gastric lesions than to
colorectal, and is difficult to distinguish from benign abnormalities,
such as erosion or inflammation [1,2]. Our results are in accordance to other previous reports [1,2]. Moreover, there is limited international experience in endoscopic tissue characterization of such early duodenal lesions [1,2].
Magnification endoscopy combined with nARGHow band
imaging (NBI-ME) is a novel advanced imaging technology with promising
results regarding the accurate diagnosis of early gastric and colorectal
cancer [10-12,19]. Details of this system have been published elsewhere [20,21].
NBI magnification improved the optical identification of early cancer
in stomach and colorectum revealing abnormal mucosal microsurface and
microvascular patterns, which have been classified, while permitted
endoscopic prediction of histology and determination of tumor margins.
NBI-ME enhances microvascular architecture and microsurface structure of
the superficial GI mucosa and based on these findings a real-time,
reliable differential diagnosis between regular (normal) and irregular
(cancerous) pattern can be made, according to several report [10-13,19,22, 23].
Moreover, there are currently in use standardized NBI-ME classifications for gastric [10,13,19] and colorectal neoplasms [11,12],
however no such classification has been reported for duodenal lesions.
In view of absence of specific NBI-ME classification for duodenal
lesions, and in combination with the endoscopic appearance to resemble
more to gastric lesions, we used the standardized NBI-ME classifications
for gastric lesions for endoscopic tissue characterization of duodenal
lesions as well. We used the four-type NBI-ME classification (fine
network, intra-lobular loop pattern (ILL)-1, ILL-2 and corkscrew
patterns) previous published by Yokoyama et al. [10] and the more recent modification after acetic acid spray published by Eleftheriadis et al. [13],
and unexpectedly and to our big surprise these classifications worked
absolutely for endoscopic tissue characterization of this particular
duodenal lesion as well. These classifications permitted not only the
endoscopic diagnosis of early duodenal cancer in real-time, but also
make endoscopic prediction of histology (well differentiated versus
undifferentiated duodenal adenocarcinomas), based on NBI-ME findings [10,24].
Interestingly, in the depressed type '0-IIc' duodenal lesion shown in Figures 1-2,
NBI at the maximum magnification showed abnormal mucosal microsurface
pattern absolutely suitable to inter-lobular loop pattern 1 (ILL-1),
which was corresponded to well-differentiated type mucosal duodenal
adenocarcinoma, and finally proved by histopathology of the resected ESD
specimen. These results are in accordance to the above-mentioned
classification by Yokoyama et al. [10].
Another interesting finding of the present study is
that NBI-ME after acetic acid spray was superior to NBI-ME alone in
obtaining high-quality endoscopic images of this early duodenal cancer,
showing increased intensity of villous pattern perfectly reflecting to
well-differentiated duodenal adenocarcinoma, as it is shown in Figures 2D-2F and
proved by final histopathological examination of the ESD specimen.
Endoscopic resection, either EMR or ESD are the treatment of choice for
early duodenal neoplasms as well, however these procedures in duodenum
are more challenging and demanding, with higher risk of complications,
such as perforation or bleeding, even in experts hands [1,2].
FAP is associated with an increased risk of duodenal
adenomas or carcinomas and these patients should be under routine
surveillance [2].
However, endoscopic optical identification of NADN in FAP patients, is
demanding, necessitating incorporation of more sophisticated advanced
endoscopic technology in routine screening, mainly cup-endoscopy, NBI-ME
in combination with acetic acid spray and use of the standardized
NBI-ME classifications [1,2,13].
Endoscopic histology in real time by NBI-ME could provide a higher
diagnostic value for surveillance of NADN in FAP patients according to
rare reports [2].
Preoperative evaluation is important to identify lesions in early
curable stage, which can be treated by endoscopic resection alone, as in
all our cases. Moreover, the risk of overlooked small duodenal adenomas
in FAP that could be progressed to cancer cannot be ruled out
completely, while the necessity for closer follow-up in FAP with NADN is
not known. The rarity of early NADNs, in combination with the limited
international data with these lesions, makes our study interesting for
publication.
In conclusion, NBI-ME in combination with acetic acid
spray is a safe, reliable and effective method for accurate optical
identification and endoscopic prediction of histology of primary NADN
(adenomas or carcinoma). NBI magnification endoscopy was superior to
conventional endoscopic methods in providing accurate, real-time,
endoscopic tissue characterization of type '0-IIc' early duodenal
cancer. Furthermore, the standardized NBI-ME classifications for early
gastric cancer were absolutely useful and worked for endoscopic
histological diagnosis of primary nonampullary duodenal lesions as well.
Further studies and more experience in such novel diagnostic techniques
are necessary.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php




Comments
Post a Comment