Are we Endoscopic Treatment of GERD and Case Report: Successful Anti-Reflux Mucosectomy (ARMS) For Endoscopic Treatment of PPI-Resistant GERD in A 24-Years-Old Greek
Authored by Nikolas Eleftheriadis
Abstract
Aim:To present an update of the endoscopic therapies of GERD and to discuss further developments.
Methods:A PubMed search was
performed. Also, we report our experience from the successful
application of antireflux mucosectomy (ARMS), a recent endoscopic
technique for GERD, in a young Greek female with refractory to PPIs GERD
and severe respiratory symptoms, who showed excellent long-term results
one-year after ARMS, with low morbidity, hospitalization time and cost.
Results: Currently, there are 3
commonly employed anti-reflux endoluminal procedures: a) fundoplication
or suturing techniques (EndoCinch, NDO, and EsophyX), b) intramural
injection or implant techniques (enhancing lower esophageal sphincter
(LES) volume and/or strengthening compliance of the LES (Enteryx and
Gatekeeper), and c) radiofrequency energy deliver to LES and cardia
(Stretta). Although all three techniques were able to improve symptoms,
the quality of life, PPI use and esophageal acid reduction were
unremarkable. Endocinch and Stretta are safe outpatient procedures.
Polymer injection (Enteryx) and gel prosthesis implantation (Gatekeeper)
were recalled for severe complications and lack of efficacy,
respectively. No single endoscopic modality has been yet proved or
accepted as the endoscopic therapy of choice for GERD. Recently,
antireflux mucosectomy (ARMS), based on natural scar formation after
healing of the mucosal defect, has been described as miniinvasive,
effective endoscopic treatment for PPI-resistant GERD, with no need of
insertion or implantation of any foreign instruments into the lower
esophagus.
Conclusion: Endotherapy has shown
the potential to treat uncomplicated GERD. However, some early
procedures have failed or proven unsafe. Further developments and
studies are necessary to determine what modifications to these
techniques are required to produce optimal efficacy and durability.
Finally, ARMS showed promising results as the minimally invasive,
endoscopic treatment for GERD in pioneering centers. However, long-term
results from greater number of patients are necessary and awaited.
Endoscopic Treatment of GERD
Background
Aim: To present an update of the endoscopic therapies of GERD and to discuss further developments.
Methods: A PubMed search was performed for <>, <>, <>, <>, <> for GERD. Also, we report our experience from the successful application of antireflux mucosectomy (ARMS [1]), a
recent endoscopic technique for GERD, in a young Greek female
with refractory to PPIs GERD and severe respiratory symptoms,
who showed excellent long-term results one-year after ARMS,
with low morbidity, hospitalization time and cost.
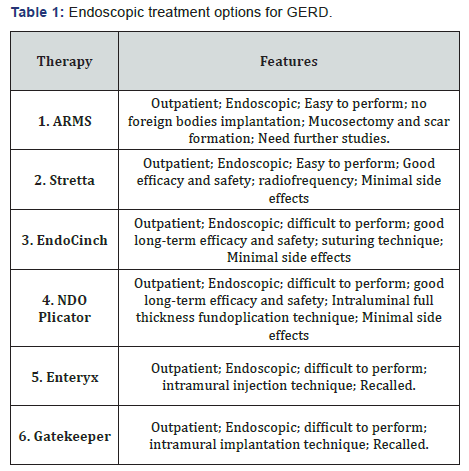
Results: Currently, there are [2,3] commonly employed
anti-reflux endoluminal procedures (Table 1): a) fundoplication
or suturing techniques (EndoCinch [2], NDO [3], and EsophyX
[4]), b) intramural injection or implant techniques (enhancing
lower esophageal sphincter (LES) volume and/or strengthening
compliance of the LES (Enteryx and Gatekeeper) [5,6], and c)
radiofrequency energy deliver to LES and cardia (Stretta [7,8]).
Although all three techniques were able to improve
symptoms, the quality of life and PPI use, esophageal acid
reduction were unremarkable. Endocinch and Stretta are safe
outpatient procedures [2,6,8]. Concerns about the durability of
Endocinch have risen [9], Polymer injection (Enteryx [4]) and
gel prosthesis implantation (Gatekeeper [6]) were recalled for
severe complications and lack of efficacy, respectively.
Uncontrolled studies have reported promising clinical
results on the short to intermediate term for most endoscopic
GERD procedures, but the placebo effect remained unknown
[9], while no single endoscopic modality has been yet proved or
finally accepted as the more efficacious or is considered as the
endoscopic therapy of choice.
Recently, antireflux mucosectomy (ARMS) [1], based on
natural scar formation after healing of the mucosal defect, has
been described as miniinvasive, effective endoscopic treatment
for PPI-resistant GERD, without large hiatal hernia, with no need
of insertion or implantation of any foreign instruments into the
lower esophagus.
Case Report
We report on a 25-years-old female with 3-years history of PPIresistant
GERD, with esophagitis Los Angeles (LA) classification
type II, serious respiratory symptoms and histological findings of
non-dysplastic BARGHett esophagus successfully treated by ARMS.
Patient continued to have respiratory and reflux symptoms
despite long-term high PPI-doses (pantoprazole 40mg twice
daily), with significant deterioration of her quality of life and
decided to go further to either surgical fundoplication or other
endoscopic treatment.
ARMS proposed as less invasive endoscopic treatment,
with low recovery time, which was accepted and subsequently
performed in the endoscopy department, under conscious
sedation. Piecemeal endoscopic mucosal resection with
cup (EMR-C) technique [10] was used to complete a semicircumferential
ARMS, including one cm above and two cm below
the gastro esophageal junction (GEJ) and with no more than 2/3
of the cardia circumference to prevent severe stenosis, according
to initial description by Inoue, et al. [1] (Figure 1 A-C).
Four snares [10] were used and total eight mucosectomy
pieces were removed. No major acute or late complications
were reported, particularly no bleeding or perforation. Patient
recovered uneventfully and discharged one day after. She began
liquid diet the day after and gradually increased to soft diet. She
returned to her usual activities three days later. She complained
of mild chest pain during the first week after ARMS, easilycontrolled by common analgesics and received high PPI-doses
for 40 days. Control endoscopy one month after ARMS showed
excellent healing and closure of the GEJ without any sign of
stenosis (Figure 1D). During one-year follow-up post-ARMS,
the patient is asymptomatic, reported no GERD or respiratory
symptoms and stopped the PPIs.
According to our experience, from the successful application
of ARMS, although in only one patient, we consider ARMS as easy,
safe and effective, endoscopic treatment for PPI-resistant GERD,
with low morbidity, hospitalization time and cost, with excellent
outcome remained in long-term. However, longer follow-up and
greater number of patients from pioneering centers are awaited
for this promising, miniinvasive, endoscopic treatment for GERD.
Conclusion
Endotherapy has shown the potential to treat uncomplicated
GERD. However, some early procedures have failed or proven
unsafe. Further developments and studies are necessary to
determine what modifications to these techniques are required
to produce optimal efficacy and durability. Finally, ARMS
showed promising results as the minimally invasive, endoscopic
treatment for GERD in pioneering centers, without the need of
insertion or implantation of any foreign instruments into the
lower esophagus.
To Know More About Advanced Research in Gastroenterology &
Hepatology Journal
click on:
https://juniperpublishers.com/argh/index.php
https://juniperpublishers.com/argh/index.php





Comments
Post a Comment